Table of Contents
ToggleWhat is sinusitis?
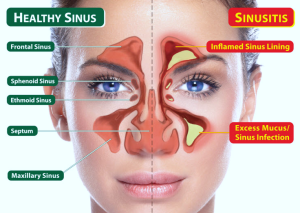
Sinusitis is a condition affecting the paranasal sinuses, characterized by inflammation of the sinus linings, often triggered by viral, bacterial, or fungal infections, along with other factors such as allergies or anatomical abnormalities. Common symptoms include facial pain and pressure, particularly around the forehead, cheeks, and eyes, exacerbated by bending forward, as well as nasal congestion and discharge, which may vary in color and consistency. These symptoms arise due to increased mucus production and impaired drainage from the sinuses, leading to difficulty breathing through the nose.
Types of Sinusitis
- Acute Sinusitis: Acute sinusitis typically lasts less than four weeks and is often caused by viral infections, such as the common cold. It may also result from bacterial infections or allergies. Symptoms include facial pain, nasal congestion, headaches, and thick nasal discharge.
- Chronic Sinusitis: Chronic sinusitis persists for more than twelve weeks and may be caused by persistent inflammation, recurrent infections, nasal polyps, or structural abnormalities. Symptoms are similar to those of acute sinusitis but may be less severe and more persistent, often accompanied by fatigue and a reduced sense of smell.
- Sub-acute Sinusitis: Sub-acute sinusitis lasts between four and twelve weeks and shares characteristics of both acute and chronic sinusitis. Symptoms may be more prolonged than acute sinusitis but less severe than chronic sinusitis.
- Recurrent Sinusitis: Recurrent sinusitis is characterized by multiple episodes of acute sinusitis within a year, with symptoms resolving between episodes. It may be associated with underlying conditions such as allergies, nasal polyps, or immune system disorders.
- Allergic Fungal Sinusitis (AFS): AFS is a type of chronic sinusitis caused by an exaggerated immune response to fungal allergens, typically occurring in individuals with a history of allergic rhinitis or asthma. It is characterized by nasal polyps, thick fungal debris in the sinuses, and persistent symptoms despite treatment.
Causes of Sinusitis
- Viral Infections: Common viral infections, such as the common cold or influenza, can cause inflammation of the sinus linings, leading to acute sinusitis. These viruses can impair the normal function of the sinuses and contribute to symptoms such as nasal congestion, facial pain, and headaches.
- Bacterial Infections: Bacterial infections can occur as a complication of viral sinusitis or independently and are more commonly associated with acute or chronic sinusitis. Bacterial sinusitis often develops when the sinus cavities become blocked, allowing bacteria to multiply and cause infection. Common bacterial pathogens include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.
- Allergic Reactions: Allergic sinusitis, also known as allergic rhinosinusitis, can result from an exaggerated immune response to allergens such as pollen, dust mites, animal dander, or mold spores. Exposure to these allergens triggers inflammation in the nasal passages and sinuses, leading to symptoms characteristic of sinusitis, including nasal congestion, sneezing, and facial pressure.
- Nasal Polyps: Nasal polyps are noncancerous growths that can develop in the nasal passages or sinuses, obstructing normal drainage and ventilation. Chronic inflammation associated with conditions such as allergic rhinitis, asthma, or chronic sinusitis can contribute to the formation of nasal polyps, exacerbating symptoms of sinusitis and increasing the risk of recurrent infections.
- Structural Abnormalities: Structural abnormalities in the nasal passages or sinuses, such as a deviated septum, narrow sinus openings, or nasal bone spurs, can impede proper drainage and ventilation, predisposing individuals to sinusitis. These abnormalities may be present at birth or result from trauma, previous surgeries, or chronic inflammation.
- Immune System Disorders: Disorders affecting the immune system, such as immunodeficiency syndromes or autoimmune diseases like granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis), can compromise the body’s ability to fight off infections and maintain normal immune responses, increasing susceptibility to sinusitis.
- Environmental Irritants: Exposure to environmental pollutants, cigarette smoke, chemical fumes, or other airborne irritants can irritate the nasal passages and sinuses, leading to inflammation and congestion. Prolonged exposure to these irritants can exacerbate the symptoms of sinusitis and contribute to the development of chronic sinusitis.
Predisposing Factors for Sinusitis
- Respiratory Infections: Patients with a history of frequent respiratory infections, such as the common cold or influenza, are at an increased risk of developing sinusitis. These infections can lead to inflammation of the sinus linings and impair normal sinus drainage, predisposing to sinusitis.
- Allergies: Allergic rhinitis, also known as hay fever, is a common predisposing factor for sinusitis. Exposure to allergens such as pollen, dust mites, or animal dander triggers an inflammatory response in the nasal passages and sinuses, leading to swelling and obstruction of the sinus openings.
- Nasal Abnormalities: Structural abnormalities in the nasal passages, such as a deviated septum, nasal polyps, or narrow sinus openings, can impede proper sinus drainage and ventilation, increasing the risk of sinusitis. These abnormalities may be present from birth or develop as a result of trauma or previous surgeries.
- Immune System Disorders: Conditions that compromise the immune system, such as HIV/AIDS, diabetes, or autoimmune diseases, can weaken the body’s ability to fight off infections and maintain normal immune responses, making individuals more susceptible to sinusitis.
- Cystic Fibrosis: Cystic fibrosis is a genetic disorder that affects the lungs and digestive system, leading to thick, sticky mucus production. This abnormal mucus can block the sinus openings and impair sinus drainage, predisposing individuals with cystic fibrosis to recurrent sinus infections.
- Environmental Factors: Exposure to environmental irritants such as cigarette smoke, air pollution, or chemical fumes can irritate the nasal passages and sinuses, leading to inflammation and increasing the risk of sinusitis. Prolonged exposure to these irritants can exacerbate symptoms and contribute to the development of chronic sinusitis.
- Immunodeficiency: Individuals with impaired immune function, either due to genetic disorders, chemotherapy, or long-term steroid use, have a higher risk of developing sinusitis. A weakened immune system makes it more difficult for the body to fight off infections, including those that affect the sinuses.
- Previous Sinus Surgery: Individuals who have undergone previous sinus surgeries may have altered sinus anatomy or scarring that affects sinus drainage and ventilation, predisposing them to recurrent sinus infections. Additionally, surgical interventions can disrupt normal mucociliary clearance mechanisms, increasing the risk of postoperative sinusitis.
Pathophysiology
Sinusitis, characterized by inflammation of the mucous membranes lining the paranasal sinuses, stems from a multifaceted interplay of various physiological factors. Firstly, obstruction of sinus outflow tracts plays a pivotal role in its pathophysiology.
The sinuses naturally produce mucus that drains through small openings called ostia into the nasal cavity. However, when these ostia become blocked due to inflammation, swelling, or structural abnormalities, mucus accumulates within the sinuses, fostering an environment conducive to bacterial or viral growth.
Concomitant mucosal inflammation further complicates the condition. Triggered by infections, allergies, or irritants, the mucous membranes lining the sinuses undergo inflammation, leading to an augmented production of mucus.
This exacerbates sinus congestion and obstruction, exacerbating the symptoms of sinusitis. Additionally, impaired mucociliary clearance, a process reliant on cilia lining the sinuses to sweep mucus and debris outward, further contributes to obstruction and exacerbates the condition.
Microbial infection, particularly in cases of bacterial sinusitis, adds another layer of complexity. Opportunistic pathogens capitalize on the stagnant mucus within the sinuses, leading to infection and inflammation.
Similarly, viral infections can predispose individuals to sinusitis by disrupting normal sinus function and fostering bacterial colonization. The resulting damage to the sinus mucosa, coupled with edema or swelling of the sinus linings, perpetuates obstruction and impairs sinus drainage, reinforcing the cycle of inflammation and infection.
In severe or untreated cases, sinusitis can extend beyond the paranasal sinuses, involving nearby structures such as the orbit, the brain, or the facial bones. Such complications, albeit rare, pose significant health risks and necessitate prompt medical intervention.
Overall, sinusitis emerges as a complex interplay of inflammation, obstruction, and microbial infection, underpinning the characteristic symptoms of facial pain, nasal congestion, and nasal discharge.
Effective management entails addressing underlying causes, mitigating inflammation, promoting sinus drainage, and treating associated infections to alleviate symptoms and prevent complications.
Signs and Symptoms
Sinusitis manifests through a spectrum of signs and symptoms indicative of inflammation and obstruction within the paranasal sinuses.
- Facial Pain or Pressure: Patients commonly experience discomfort or pressure sensations in areas surrounding the affected sinuses, such as the forehead, cheeks, and around the eyes. This pain arises due to the buildup of pressure within the sinuses caused by inflammation and swelling of the sinus linings.
- Nasal Congestion or Obstruction: Nasal congestion or blockage is a hallmark symptom of sinusitis, resulting from the swelling of the mucous membranes lining the nasal passages and sinuses. This obstruction impedes the flow of air through the nasal passages, making breathing difficult.
- Thick Nasal Discharge: Sinusitis often leads to the production of thick nasal discharge, which may vary in color from clear to yellowish-green or even bloody. This discharge consists of mucus and inflammatory cells, indicative of the body’s immune response to infection or irritation within the sinuses.
- Headache: Headache, particularly localized over the affected sinus areas, is a common symptom of sinusitis. This headache arises due to the increased pressure within the sinuses caused by inflammation and congestion, leading to pain and discomfort.
- Reduced Sense of Smell or Taste: Sinusitis can impair the sense of smell, known as anosmia, or alter the perception of taste, known as dysgeusia. This occurs due to inflammation and swelling of the sinus linings, which can obstruct the olfactory nerves responsible for smell and taste perception.
- Cough: Some individuals with sinusitis may develop a cough, which can be dry or productive. This cough arises as a result of postnasal drip, where excess mucus drips down the back of the throat from the inflamed sinuses, irritating the throat and triggering coughing reflexes.
- Sore Throat: Sinusitis may cause throat discomfort or soreness, particularly if postnasal drip irritates the throat tissues. This symptom is often accompanied by a persistent sensation of throat irritation or tickling.
- Fatigue: Sinusitis can contribute to feelings of fatigue or malaise, as the body expends energy to combat the underlying inflammation and infection. Additionally, disrupted sleep patterns due to nasal congestion or discomfort can further exacerbate feelings of fatigue.
- Ear Pressure: Some individuals with sinusitis may experience sensations of fullness or pressure in the ears, known as ear barotrauma. This occurs due to the close anatomical relationship between the sinuses and the Eustachian tubes, which regulate pressure within the middle ear.
- Fever: In cases of acute sinusitis, individuals may develop a fever as the body mounts an immune response to the underlying infection. Fever is a systemic manifestation of inflammation and infection, indicating an elevated body temperature in response to pathogens invading the sinuses.
Medical Management
History
- Symptom Assessment: Ask about the duration and nature of symptoms such as facial pain or pressure, nasal congestion, nasal discharge, headache, cough, and fever.
- Onset and Progression: Ask whether symptoms developed suddenly (acute sinusitis) or have been persistent or recurrent (chronic sinusitis).
- Triggers and Aggravating Factors: Ask the patient about potential triggers such as recent respiratory infections, allergies, environmental exposures, or changes in altitude.
- Past Medical History: Evaluate for a history of sinusitis, allergies, nasal polyps, asthma, immune disorders, or structural abnormalities in the nasal passages.
- Medication Use: Assess for current or recent use of medications, including antibiotics, decongestants, nasal steroids, or antihistamines.
Physical Examination
- Nasal Examination: Inspect the nasal passages for any signs of inflammation, swelling, or discharge. Evaluate the nasal mucosa for erythema, edema, or the presence of nasal polyps.
- Sinus Palpation: Palpate the sinus areas over the forehead, cheeks, and around the eyes for tenderness or pain, indicative of sinus inflammation.
- Oropharyngeal Examination: Assess the oropharynx for signs of postnasal drip, such as mucous pooling or cobblestoning of the posterior pharyngeal wall.
- Otoscopic Examination: Examine the tympanic membranes for signs of middle ear effusion or congestion, which may indicate Eustachian tube dysfunction secondary to sinusitis.
- Temperature Measurement: Obtain a temperature reading to assess for fever, which may accompany acute sinusitis in cases of bacterial or severe viral infections.
- Lymph Node Evaluation: Palpate cervical lymph nodes for enlargement or tenderness, which may indicate reactive lymphadenopathy secondary to sinusitis or underlying infection.
Investigations
- Nasal Endoscopy: Nasal endoscopy involves the use of a thin, flexible tube with a camera and light at its tip to visualize the nasal passages and sinuses. It allows direct examination of the nasal mucosa, detection of nasal polyps, and assessment of sinus anatomy, aiding in the diagnosis and management of sinusitis.
- Imaging Studies:
- Sinus X-rays: Plain radiographs of the paranasal sinuses may be obtained to assess for signs of sinusitis, such as air-fluid levels, mucosal thickening, or opacification of the sinuses. However, sinus X-rays have limited sensitivity and specificity compared to other imaging modalities.
-
-
- Computed Tomography (CT) Scan: CT imaging provides detailed cross-sectional images of the sinuses, allowing for accurate assessment of sinus anatomy, mucosal inflammation, and complications of sinusitis. CT scans are particularly useful for diagnosing chronic or complicated sinusitis.
-
-
-
- Magnetic Resonance Imaging (MRI): MRI may be indicated in cases where CT imaging is contraindicated or to evaluate for intracranial or orbital complications of sinusitis. MRI provides excellent soft tissue contrast but is less commonly used than CT for sinus imaging.
-
- Nasal Culture: Nasal swabs or sinus aspirates may be obtained for culture and sensitivity testing in cases of severe or refractory sinusitis. This helps identify the causative pathogens, guide antibiotic selection, and determine antibiotic susceptibility patterns.
- Allergy Testing: Allergy testing, including skin prick tests or serum IgE levels, may be performed in individuals with suspected allergic rhinosinusitis. Identifying specific allergens that trigger symptoms can guide allergen avoidance strategies and targeted allergy treatment.
- Nasal Cytology: Nasal cytology involves obtaining a nasal smear or biopsy sample to examine nasal epithelial cells under a microscope. It may be useful in identifying eosinophils or other inflammatory cells characteristic of allergic or eosinophilic sinusitis.
- Sinus Aspiration: Sinus aspiration involves the insertion of a needle into the sinus cavity to aspirate fluid or purulent material for microbiological analysis. This invasive procedure is typically reserved for cases of severe or complicated sinusitis where a definitive diagnosis is needed or when other diagnostic methods have failed.
Treatment of Sinusitis
- Warm Compress Application: Applying a warm, moist cloth to the face several times a day can help alleviate facial pain and pressure associated with sinusitis. The warmth helps to soothe inflammation and promote sinus drainage, providing symptomatic relief.
- Steam Inhalation: Inhaling steam three to four times a day, such as by sitting in the bathroom with hot water running, can help to moisten and soothe the nasal passages. Steam inhalation helps to loosen mucus, alleviate nasal congestion, and promote sinus drainage, providing symptomatic relief.
- Nasal Saline Spray and Humidifiers: Using nasal saline spray several times a day and employing humidifiers in the home can help to keep the nasal passages moist and facilitate sinus drainage. Saline irrigation helps to flush out mucus and debris from the sinuses, while humidifiers add moisture to the air, reducing nasal dryness and congestion.
- Antibiotics:
- First-Line Antibiotics: Commonly prescribed first-line antibiotics for sinusitis include amoxicillin, erythromycin, and co-trimoxazole. These antibiotics are effective against bacterial infections commonly associated with sinusitis.
-
- Second-Line Antibiotics: If first-line antibiotics are ineffective or if the infection is suspected to be caused by resistant bacteria, second-line antibiotics such as cephalosporins (e.g., cefuroxime, ceftriaxone, and cephalexin) may be prescribed.
- Decongestants: Oral and topical decongestant agents are used to reduce swelling of the nasal mucosa and nasal polyps, thereby improving sinus drainage and alleviating nasal congestion. Decongestants help to shrink swollen nasal tissues, allowing for easier breathing and improved airflow.
- Hydration: Drinking plenty of fluids helps to thin mucus secretions, making them easier to expel and promoting sinus drainage. Adequate hydration also helps to maintain overall health and supports the body’s immune response to infection.
- Surgical Intervention:
- Endoscopic Surgery: Endoscopic sinus surgery may be recommended to correct structural deformities that obstruct the openings (ostia) of the sinuses. This minimally invasive procedure involves inserting an endoscope through the nostrils to visualize and correct anatomical abnormalities.
-
- Polypectomy: Excising and cauterizing nasal polyps may be necessary to improve sinus drainage and alleviate symptoms of sinusitis. This surgical procedure involves removing polyps from the nasal passages or sinuses to restore normal airflow.
-
- Septoplasty: Correcting a deviated septum through septoplasty surgery can help improve airflow through the nasal passages and promote sinus drainage.
-
- Sinus Drainage: In cases of severe sinusitis with abscess formation or persistent symptoms despite medical treatment, surgical intervention may involve incision and drainage of the affected sinus to aerate the sinus cavity and remove any pus or debris. Additionally, surgical removal of tumors obstructing sinus drainage may be necessary to alleviate symptoms and prevent complications.
Nursing Management
Aims
- To alleviate sinusitis symptoms such as facial pain, nasal congestion, headache, and fever to improve patient comfort and quality of life.
- To minimize the risk of complications associated with sinusitis, including orbital cellulitis, meningitis, and intracranial abscess, through early detection and intervention.
- To promote sinus drainage and clearance of mucus, allergens, and infectious agents to reduce congestion and facilitate recovery.
- To implement measures to prevent the recurrence of sinusitis episodes by addressing predisposing factors, optimizing treatment, and promoting patient education and self-management strategies.
Infection Prevention
- Encourage patients and caregivers to practice frequent handwashing with soap and water or alcohol-based hand sanitizers to prevent the spread of infectious agents. Rationale: Proper hand hygiene reduces the transmission of bacteria and viruses, minimizing the risk of secondary infections and promoting overall health.
- Implement appropriate isolation precautions, such as droplet precautions, for patients with contagious sinus infections to prevent the spread of respiratory pathogens to others. Rationale: Isolation precautions help contain infectious agents, reducing the risk of transmission to healthcare workers, other patients, and visitors.
- Ensure thorough disinfection of shared items and surfaces in patient care areas to reduce the risk of cross-contamination and infection transmission. Rationale: Disinfection of frequently touched surfaces helps prevent the spread of infectious agents, maintaining a clean and safe environment for patients and healthcare providers.
- Educate patients and visitors on proper respiratory etiquette, including covering the mouth and nose when coughing or sneezing, to minimize the dissemination of respiratory droplets containing infectious agents. Rationale: Respiratory etiquette reduces the spread of respiratory pathogens, preventing the transmission of sinusitis-causing agents to others in the healthcare setting.
Environment
- Ensure adequate ventilation and air circulation in patient care areas to minimize exposure to environmental irritants and allergens that may exacerbate sinusitis symptoms. Rationale: Improved air quality reduces the concentration of airborne pollutants and allergens, creating a more comfortable and conducive environment for patients with sinusitis.
- Maintain optimal humidity levels in patient rooms using humidifiers to prevent nasal dryness and irritation, which can worsen sinusitis symptoms.Rationale:Adequate humidity helps keep nasal passages moist, facilitating mucociliary clearance and promoting sinus drainage, thereby relieving congestion and discomfort.
- Identify and minimize exposure to allergens in the patient’s environment, such as dust mites, pet dander, or mold, which can trigger allergic rhinosinusitis. Rationale: Minimizing exposure to allergens reduces nasal inflammation and irritation, alleviates sinusitis symptoms, and improves patient comfort.
- Maintain a comfortable room temperature for patients, avoiding extremes of heat or cold that may exacerbate sinusitis symptoms. Rationale: Extreme temperatures can irritate the nasal passages and exacerbate sinus congestion, discomfort, and inflammation. Maintaining a comfortable temperature promotes patient comfort and symptom relief.
Observation
- Conduct frequent assessments of sinusitis symptoms, including facial pain, nasal congestion, headache, and fever, to evaluate the patient’s condition and response to treatment.Rationale: Regular symptom monitoring allows for early detection of worsening symptoms or complications, enabling timely intervention and preventing the progression of sinusitis.
- Be vigilant for signs of complications such as orbital cellulitis, meningitis, or intracranial abscess, particularly in severe or refractory cases of sinusitis. Promptly report any concerning findings to the healthcare team. Rationale: Early recognition of complications allows for timely intervention and prevents potentially life-threatening sequelae associated with sinusitis, minimizing morbidity and mortality.
- Assess the patient’s emotional well-being and psychological response to sinusitis symptoms, such as frustration, anxiety, or depression, and provide appropriate support and counseling as needed. Rationale: Sinusitis can significantly impact quality of life and emotional health, particularly in cases of chronic or recurrent sinusitis. Addressing psychological distress promotes holistic patient care and enhances coping mechanisms.
- Provide comprehensive education about sinusitis to a patient, including its causes, symptoms, treatment options, and self-care strategies, to empower patients to actively participate in their management and recovery. Rationale:Patient education fosters patient autonomy, promotes treatment adherence, and facilitates informed decision-making, leading to better outcomes and patient satisfaction.
Hygiene
- Educate a patient on proper nasal hygiene practices, such as saline nasal irrigation and gentle blowing of the nose, to promote sinus drainage and alleviate congestion. Rationale:Nasal hygiene practices help remove excess mucus, allergens, and irritants from the nasal passages, reducing inflammation and improving sinus symptoms.
- Encourage the patient to engage in regular oral hygiene practices, including brushing teeth and rinsing with mouthwash, to prevent oral bacterial colonization and reduce the risk of secondary sinus infections. Rationale: Maintaining oral hygiene helps minimize the spread of bacteria from the mouth to the sinuses, preventing secondary infections and supporting overall sinusitis management.
- Tell the patient about the importance of maintaining skin integrity, particularly around the nasal area, to prevent skin breakdown and minimize the risk of secondary infections. Rationale: Intact skin serves as a barrier against microbial invasion, reducing the risk of skin infections and complications in patients with sinusitis.
- Ensure cleanliness and sanitation of patient care areas, including bed linens, personal hygiene items, and medical equipment, to prevent contamination and reduce the risk of infection transmission. Rationale: Environmental hygiene measures help create a safe and hygienic environment for patients, minimizing the risk of healthcare-associated infections and promoting recovery from sinusitis.
Nutrition
- Encourage the patient about the importance of adequate fluid intake, including water, herbal teas, and clear broths, to maintain hydration and help thin mucus secretions, making them easier to expel. Rationale: Proper hydration helps loosen thick mucus, facilitating its removal from the sinuses and promoting sinus drainage, thereby relieving congestion and discomfort.
- Give a patient a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to support overall immune function and promote healing. Rationale: A nutrient-rich diet provides essential vitamins, minerals, and antioxidants necessary for immune system function, aiding in the body’s ability to fight off infections and recover from sinusitis.
- Educate a patient on identifying and avoiding trigger foods that may exacerbate sinusitis symptoms, such as dairy, gluten, or spicy foods. Rationale: Eliminating trigger foods reduces the risk of triggering allergic reactions or inflammation in the nasal passages, contributing to symptom relief and improved management of sinusitis.
- Supplemental Nutrition: Consider providing nutritional supplements or meal replacement options for patients with decreased appetite or difficulty eating due to sinusitis symptoms. Rationale: Supplemental nutrition helps ensure adequate nutrient intake, particularly during periods of decreased appetite or inability to consume regular meals, supporting overall health and recovery.
Elimination
- Encourage a patient to maintain regular bowel habits through dietary fiber intake, hydration, and physical activity to prevent constipation, which can exacerbate sinusitis symptoms. Rationale: Constipation can lead to increased intra-abdominal pressure, which may worsen sinus congestion and discomfort. Maintaining regular bowel habits promotes overall comfort and well-being.
- Provide assistance to a patient with toileting as needed, particularly for patients with limited mobility or those recovering from sinusitis-related surgery, to ensure optimal elimination and prevent complications such as urinary retention. Rationale: Assisting patients with toileting promotes comfort, maintains hygiene, and reduces the risk of urinary retention or urinary tract infections, supporting overall recovery from sinusitis.
- Monitor the patient’s urinary output and assess for signs of urinary retention or urinary tract infections in patients at risk, such as those receiving opioid pain medications or experiencing urinary symptoms. Rationale: Monitoring urinary output helps identify urinary retention or infection early, enabling prompt intervention and preventing complications in patients with sinusitis.
- Educate the patient on bladder health, including strategies to prevent urinary tract infections and promote bladder emptying, to empower patients to manage their urinary function during sinusitis recovery. Rationale:Bladder health education empowers patients to recognize and address urinary symptoms, reducing the risk of complications and promoting overall well-being during sinusitis management.
Medicine
- Educate a patient on the importance of adhering to prescribed medication regimens, including antibiotics, decongestants, and pain relievers, to effectively manage sinusitis symptoms and prevent complications. Rationale: Adherence to medication regimens ensures optimal therapeutic outcomes, reduces the risk of treatment failure or relapse, and promotes timely resolution of sinusitis.
- Instruct a patient on the correct administration technique for medications, including nasal sprays, inhalers, and oral medications, to maximize their effectiveness and minimize side effects. Rationale:Proper medication administration ensures accurate dosing and delivery of medications to the affected areas, enhancing their therapeutic benefits and improving symptom management.
- Give appropriate pain management interventions, such as over-the-counter analgesics or prescription pain medications, to alleviate facial pain, headaches, and discomfort associated with sinusitis. Rationale: Effective pain management enhances patient comfort, improves quality of life, and promotes restful sleep, facilitating recovery from sinusitis.
- Educate a patient on the importance of completing the full course of antibiotics as prescribed, even if symptoms improve before the medication is finished, to prevent antibiotic resistance and recurrent infections. Rationale: Antibiotic stewardship helps preserve the effectiveness of antibiotics, reduces the risk of antibiotic resistance, and minimizes the incidence of recurrent sinusitis episodes.
Advice at Discharge
- Advise a patient to minimize exposure to known allergens, such as pollen, dust mites, pet dander, and mold, which can trigger allergic rhinosinusitis and exacerbate sinusitis symptoms. Rationale: Avoiding allergens reduces nasal inflammation and irritation, alleviates sinusitis symptoms, and improves overall quality of life.
- Encourage a patient to avoid exposure to environmental irritants such as cigarette smoke, air pollution, strong odors, and chemical fumes, which can aggravate sinusitis symptoms. Rationale: Avoiding environmental irritants helps reduce nasal inflammation and irritation, promoting symptom relief and enhancing sinusitis management.
- Teach a patient proper sinus irrigation techniques using saline solutions or nasal irrigation devices to promote sinus drainage and alleviate congestion. Rationale: Sinus irrigation helps remove excess mucus and allergens from the nasal passages, reducing inflammation and improving sinus symptoms.
- Emphasize the importance of follow-up appointments with healthcare providers for ongoing monitoring of sinusitis symptoms, evaluation of treatment effectiveness, and adjustment of management strategies as needed. Rationale: Regular follow-up allows for assessment of treatment response, identification of complications, and modification of management plans, optimizing patient outcomes and preventing the recurrence of sinusitis.
Preventive Measures
- Avoidance of Allergens: Advise people in the community to minimize exposure to known allergens such as pollen, dust mites, pet dander, and mold, which can trigger allergic rhinosinusitis and exacerbate sinusitis symptoms.
- Environmental Hygiene: Encourage maintaining cleanliness in living and working environments to reduce exposure to dust, pollutants, and other irritants that can irritate the nasal passages and contribute to sinusitis.
- Proper Hydration: Promote adequate fluid intake to keep mucous membranes moist and facilitate the clearance of mucus from the sinuses, reducing the risk of sinus congestion and infection.
- Nasal Irrigation: Suggest regular use of saline nasal irrigation to cleanse the nasal passages, remove allergens and irritants, and promote sinus drainage, helping to prevent sinusitis episodes.
Complications
- Brain Abscess: A brain abscess is a rare but serious complication characterized by a collection of pus within brain tissue. It often results from the spread of infection from nearby structures or through the bloodstream. Symptoms may include a severe headache, fever, nausea, vomiting, neurological deficits, and altered mental status. Prompt diagnosis and treatment with antibiotics and sometimes surgical drainage are essential to prevent neurological complications and minimize the risk of permanent brain damage or death.
- Meningitis: Meningitis is the inflammation of the meninges, the protective membranes covering the brain and spinal cord. It can be caused by bacterial, viral, or fungal infections, leading to symptoms such as severe headache, neck stiffness, fever, confusion, and sensitivity to light. Meningitis can be life-threatening, requiring immediate medical attention. Treatment typically involves antibiotics or antiviral medications, supportive care, and sometimes hospitalization for close monitoring and intravenous fluids.
- Osteomyelitis of the Facial Bones: Osteomyelitis of the facial bones refers to a bacterial infection of the bones in the face, often resulting from trauma, sinusitis, dental infections, or surgery. Symptoms may include localized pain, swelling, redness, and sometimes fever. Prompt treatment with antibiotics and surgical drainage or debridement may be necessary to prevent the spread of infection, bone destruction, and potential complications such as abscess formation or septicemia.
- Encephalitis: Encephalitis is inflammation of the brain tissue, typically caused by viral infections such as the herpes simplex virus, the West Nile virus, or certain types of bacteria. Symptoms may include fever, headache, confusion, seizures, and neurological deficits. Severe cases can lead to coma or death if not promptly diagnosed and treated with antiviral medications, supportive care, and sometimes hospitalization for monitoring and management of complications such as brain swelling.
- Ischemic Infarction: Ischemic infarction, also known as a stroke, occurs when blood flow to a part of the brain is blocked, leading to tissue damage and loss of function. Common causes include blood clots, arterial narrowing, or embolisms. Symptoms vary depending on the affected area of the brain but may include sudden weakness or paralysis on one side of the body, difficulty speaking or understanding speech, and vision changes. Immediate medical intervention, including clot-busting medications or thrombectomy, is crucial to restore blood flow and minimize brain damage.
- Subperiosteal Abscess: A subperiosteal abscess is a localized collection of pus beneath the periosteum, the outer layer of bone. It often occurs as a complication of sinusitis or dental infections, causing facial pain, swelling, and redness. Treatment typically involves antibiotics to control infection and sometimes surgical drainage to relieve pressure and prevent further bone destruction or spread of infection.
- Orbital Cellulitis: Orbital cellulitis is a serious infection of the tissues surrounding the eye within the eye socket (orbit). It usually develops as a complication of sinusitis or trauma, causing symptoms such as eye pain, swelling, redness, fever, and decreased vision. Prompt treatment with antibiotics and sometimes surgical drainage is necessary to prevent vision loss, optic nerve damage, or the spread of infection to adjacent structures such as the brain.
Read more: Medical-Surgical Nursing
Read more: Laryngitis | Causes | Signs and Symptoms | Pathophysiology | Treatment | Nursing Management








[…] Read more: Sinusitis | Causes | Pathophysiology | Signs and Symptoms | Treatment | Nursing Management […]