Table of Contents
ToggleWhat is laryngitis?
Laryngitis is an inflammation of the larynx, the part of the respiratory system commonly known as the voice box. It is typically caused by viral or bacterial infections, overuse of the vocal cords, or irritation from environmental factors such as smoke or dry air.
Two characteristics of laryngitis include hoarseness or loss of voice, which occurs due to inflammation of the vocal cords, and throat discomfort or pain, often accompanied by a dry or scratchy sensation.
Causes of Laryngitis
- Viral Infections: Viral infections are the most common cause of laryngitis, with pathogens such as measles, influenza, and the common cold often triggering inflammation of the larynx. These viruses infect the respiratory tract, leading to swelling and irritation of the vocal cords.
- Bacterial Invasion: Bacterial infections can also contribute to laryngitis, although they are typically secondary to viral infections. Bacteria such as Streptococcus or Staphylococcus may invade the larynx, causing additional inflammation and exacerbating symptoms.
- Polyps and Laryngeal Cancer: Growths such as polyps or tumors in the larynx can lead to chronic irritation and inflammation, resulting in laryngitis. Laryngeal cancer, although less common, can also cause persistent hoarseness and other symptoms characteristic of laryngitis.
- Allergies: Allergic reactions to environmental allergens, such as pollen, dust, or pet dander, can trigger inflammation of the larynx, resulting in symptoms of laryngitis. Allergic laryngitis may be accompanied by other allergy-related symptoms such as sneezing, nasal congestion, and itchy eyes.
- Voice Abuse: Overuse or misuse of the voice, such as shouting, screaming, or excessive talking, can strain the vocal cords and lead to laryngeal inflammation. This is common among individuals who use their voice extensively in professions such as teaching, singing, or public speaking.
- Exposure to Irritants: Exposure to irritants in the environment, including dust, chemicals, smoke, and other pollutants, can irritate the laryngeal mucosa and trigger inflammation. Prolonged exposure to such irritants can contribute to chronic laryngitis.
- Smoking Tobacco: Smoking tobacco is a significant risk factor for laryngitis, as the toxins and chemicals present in tobacco smoke can directly irritate and damage the laryngeal tissues. Chronic smoking can lead to chronic laryngitis and increase the risk of developing laryngeal cancer.
Signs and Symptoms
Hoarseness of Voice
- Hoarseness refers to a rough or raspy quality of voice, often characterized by changes in pitch or tone.
- It occurs due to inflammation of the vocal cords, which affects their ability to vibrate smoothly during speech.
- The inflamed vocal cords may become swollen and stiff, resulting in the characteristic hoarse sound.
Loss of Voice (Aphonia)
- Aphonia refers to the complete loss of voice, where individuals are unable to produce any sound.
- Severe inflammation of the larynx can lead to temporary or persistent aphonia, impairing the individual’s ability to communicate verbally.
- It occurs when the vocal cords are significantly swollen or inflamed, preventing them from vibrating and producing sound effectively.
Sore Throat
- Laryngitis commonly presents with a sore or scratchy throat, which may be mild to severe in intensity.
- The inflammation of the larynx and surrounding tissues can cause discomfort or pain, especially during swallowing or speaking.
- A sore throat may result from irritation of the throat tissues by inflamed vocal cords or from postnasal drip associated with laryngitis.
Dry Cough
- A dry, non-productive cough is a frequent symptom of laryngitis, often accompanied by throat irritation or tickling.
- It occurs due to the body’s reflexive response to laryngeal irritation, as the inflamed tissues trigger the cough reflex.
- The cough may worsen with speaking or exposure to irritants, such as smoke or dry air, exacerbating laryngeal inflammation.
Reasons for Signs and Symptoms
Hoarseness of Voice and Loss of Voice (Aphonia)
- Hoarseness and aphonia result from inflammation and swelling of the vocal cords, which disrupt their normal vibration and function.
- The inflammation may be caused by viral or bacterial infections, vocal cord overuse or misuse, exposure to irritants, or underlying conditions such as laryngeal polyps or cancer.
Sore Throat:
- The sore throat in laryngitis is primarily due to inflammation and irritation of the laryngeal mucosa and surrounding tissues.
- Inflammation may extend to the pharynx and upper respiratory tract, leading to throat discomfort, pain, or scratchiness.
- Postnasal drip, caused by excess mucus production and drainage from the inflamed nasal passages, can also contribute to throat irritation and soreness.
Dry Cough
- The dry cough associated with laryngitis occurs as a result of the body’s attempt to clear the airway of irritants or excess mucus.
- Laryngeal inflammation triggers the cough reflex, leading to repetitive coughing episodes that do not produce phlegm or mucus.
- Coughing may worsen with talking, laughing, or exposure to environmental factors such as dry air or airborne irritants.
Pathophysiology
Laryngitis involves inflammation of the larynx, primarily affecting the vocal cords and surrounding structures. The pathophysiology of laryngitis typically begins with exposure to irritants or pathogens that trigger an inflammatory response in the laryngeal mucosa.
Irritants such as viruses, bacteria, allergens, or environmental pollutants can cause irritation and damage to the delicate tissues of the larynx.
This leads to the release of inflammatory mediators, including histamine, cytokines, and leukotrienes, which promote vasodilation and increase vascular permeability in the affected tissues.
The influx of inflammatory cells, such as neutrophils and lymphocytes, exacerbates tissue damage and inflammation, further compromising laryngeal function.
The inflammatory process results in edema (swelling) of the laryngeal mucosa, including the vocal cords. Edema narrows the airway and impairs the normal vibration of the vocal cords, leading to changes in voice quality, such as hoarseness or loss of voice (aphonia).
Swelling may also obstruct airflow and contribute to symptoms such as difficulty breathing or stridor, particularly in severe cases.
In response to inflammation, the laryngeal mucosa may increase mucous production as a protective mechanism to lubricate and soothe irritated tissues. Excess mucous production can lead to symptoms such as throat clearing, coughing, or postnasal drip, exacerbating throat discomfort and irritation.
Inflammation and swelling of the vocal cords disrupt their normal vibration during speech and phonation. This results in hoarseness, reduced vocal range, and difficulty projecting the voice. In severe cases, complete loss of voice (aphonia) may occur due to significant swelling and inflammation of the vocal cords.
Prolonged or severe laryngeal inflammation can lead to complications such as chronic laryngitis, vocal cord nodules or polyps, or laryngeal stenosis (narrowing of the airway).
Chronic inflammation may also increase the risk of laryngeal cancer in some cases, particularly in individuals with long-term exposure to irritants such as tobacco smoke.
Medical Management
History
Onset and Duration of Symptoms
- Ask about when the symptoms of laryngitis began and how long they have been present.
- Ask if the symptoms developed suddenly or gradually over time.
Nature of Symptoms
- Ask about the specific symptoms experienced, such as hoarseness, loss of voice, sore throat, and dry cough.
- Ask about the severity of the symptoms and any factors that exacerbate or alleviate them.
Underlying Causes or Triggers
- Explore potential triggers for laryngitis, such as recent viral or bacterial infections, exposure to irritants or allergens, voice overuse, or recent changes in medication.
- Assess for any history of allergies, asthma, gastroesophageal reflux disease (GERD), or vocal cord abuse.
Occupational or environmental exposures
- Ask about the individual’s occupation and any exposure to occupational hazards such as dust, chemicals, smoke, or loud noise.
- Determine if the individual is a smoker or has regular exposure to secondhand smoke.
Medical History
- Review the individual’s past medical history, including any history of respiratory infections, chronic conditions (e.g., asthma, allergies), or previous episodes of laryngitis.
- Assess for any history of laryngeal disorders, vocal cord nodules or polyps, or laryngeal surgery.
Physical Examination
Throat Examination
- Perform a visual inspection of the throat using a tongue depressor and light source to assess for signs of inflammation, redness, or swelling of the pharynx, tonsils, and posterior pharyngeal wall.
- Look for the presence of exudate, ulcers, or lesions in the throat.
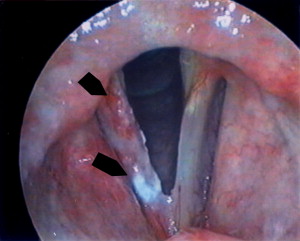
Laryngeal Examination
- Perform a laryngoscopy or indirect laryngeal examination using a laryngeal mirror or fiberoptic scope to visualize the larynx and vocal cords.
- Evaluate the appearance of the vocal cords for signs of inflammation, swelling, nodules, or other abnormalities.
- Assess vocal cord mobility and function during phonation.
Palpation of Neck
- Palpate the neck and thyroid gland to assess for tenderness, swelling, or lymphadenopathy.
- Check for the presence of enlarged cervical lymph nodes, which may indicate an underlying infection or inflammation.
Respiratory Examination
- Auscultate the lungs to assess for the presence of wheezing or diminished breath sounds, which may suggest underlying respiratory conditions such as asthma or bronchitis.
- Evaluate respiratory effort and pattern, looking for signs of respiratory distress or difficulty breathing.
General Examination
- Conduct a general physical examination to assess for signs of systemic illness or complications related to laryngitis, such as fever, malaise, or dehydration.
- Check vital signs, including temperature, pulse, blood pressure, and oxygen saturation.
Investigations
Throat Culture
- A throat culture may be performed to identify bacterial pathogens, such as Streptococcus pyogenes, in cases of suspected bacterial laryngitis.
- A throat swab is collected and cultured in a laboratory to detect the presence of bacteria.
Viral Testing
- Viral testing, such as polymerase chain reaction (PCR) or rapid antigen tests, may be conducted to identify specific viral pathogens responsible for laryngitis, particularly in cases of severe or prolonged symptoms.
Laryngoscopy
- Laryngoscopy allows direct visualization of the larynx and vocal cords using a laryngoscope, which may be rigid or flexible.
- It helps evaluate the degree of laryngeal inflammation, assess vocal cord mobility, and identify any structural abnormalities or lesions.
Imaging Studies
- Imaging studies such as neck ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI) may be indicated in cases of suspected laryngeal masses, nodules, or other structural abnormalities causing laryngitis symptoms.
Allergy Testing
- Allergy testing, including skin prick tests or blood tests (e.g., IgE antibody testing), may be recommended to identify specific allergens triggering allergic laryngitis in individuals with a history of allergies or atopy.
Laryngeal Biopsy
- A laryngeal biopsy may be performed if there is suspicion of laryngeal cancer or other serious underlying conditions. A small tissue sample is collected from the laryngeal lesion and examined under a microscope to confirm the diagnosis.
pH Monitoring
- pH monitoring, such as 24-hour esophageal pH monitoring or impedance testing, may be conducted in cases of suspected laryngopharyngeal reflux (LPR) contributing to laryngitis symptoms. It helps assess the presence and severity of acid reflux into the larynx.
Pulmonary Function Tests (PFTs)
- Pulmonary function tests may be indicated in individuals with suspected underlying respiratory conditions, such as asthma or chronic obstructive pulmonary disease (COPD), contributing to laryngitis symptoms. PFTs assess lung function and respiratory mechanics.
Blood Tests
- Blood tests, including complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), may be ordered to assess for signs of inflammation or infection in individuals with severe or prolonged laryngitis symptoms.
Voice Assessment
- Voice assessment, conducted by a speech-language pathologist (SLP) or otolaryngologist, may include voice analysis and acoustic testing to evaluate vocal quality, pitch, intensity, and resonance in individuals with persistent voice changes or vocal dysfunction.
Treatment for Laryngitis
Vocal Rest and Smoking Cessation
- Advise a patient to observe complete vocal rest to allow the inflamed vocal cords to heal effectively. This includes refraining from speaking, singing, whispering, or shouting.
- Additionally, smoking cessation is strongly recommended, as tobacco smoke can further irritate the larynx and prolong the recovery process.
Cold Steam or Aerosol Therapy
- Cold steam or aerosol therapy, such as inhaling cool mist from a humidifier or using a saline nasal spray, can help alleviate throat irritation and soothe inflamed laryngeal tissues.
- This therapy provides moisture to the airways, reducing dryness and promoting mucous clearance, which aids in symptom relief and enhances healing.
Antibiotics Only: Bacterial Origin
- Antibiotics are prescribed selectively and only if laryngitis is of bacterial origin or if there is a secondary bacterial infection present. It is essential to conduct appropriate diagnostic tests to identify the causative organism before initiating antibiotic therapy.
- Overuse of antibiotics can contribute to antibiotic resistance and may not be effective in treating viral laryngitis, which is the most common cause.
Hydration and Fluid Intake
- Adequate hydration is vital for individuals with laryngitis, as it helps maintain moisture in the throat, soothes inflamed tissues, and promotes mucous clearance.
- Patients are encouraged to drink plenty of fluids, preferably water or herbal teas, to prevent dehydration and facilitate recovery.
Throat Lozenges and Gargles
- Throat lozenges containing menthol or herbal extracts can provide temporary relief from throat discomfort and irritation.
- Gargling with warm salt water several times a day can also help reduce inflammation and alleviate soreness.
Voice Therapy
- In cases of chronic or recurrent laryngitis, referral to a speech-language pathologist for voice therapy may be beneficial.
- Voice therapy focuses on techniques to improve vocal production, reduce vocal strain, and promote vocal health through proper breathing and speaking habits.
Avoiding Irritants
- Patients are advised to avoid exposure to irritants such as smoke, air pollution, strong odors, and chemical fumes, which can exacerbate laryngitis symptoms and prolong recovery.
- This includes minimizing exposure to allergens and respiratory irritants in the environment.
Humidification
- Increasing humidity in the surrounding environment can help soothe irritated throat tissues and relieve symptoms of laryngitis.
- Using a humidifier in the bedroom or inhaling steam from a hot shower can provide temporary relief from throat dryness and discomfort.
Nutritional Support
- Maintaining a balanced diet rich in vitamins, minerals, and antioxidants is important for supporting the immune system and promoting overall health during laryngitis recovery.
- Patients are encouraged to consume nourishing foods such as fruits, vegetables, lean proteins, and whole grains.
Follow-Up and Monitoring
- Patients should be advised to follow up with their healthcare provider for evaluation of symptom resolution and assessment of vocal cord function.
- Continued monitoring may be necessary to ensure a complete recovery and to address any persistent symptoms or complications.
Nursing Management
Aims
- To alleviate symptoms such as hoarseness, sore throat, and coughing to improve patient comfort and promote restorative sleep.
- To minimize the risk of complications such as airway obstruction or secondary infections by closely monitoring the patient’s respiratory status and providing appropriate interventions.
- To reduce vocal strain and promote vocal rest, such as minimizing speaking or using a whispering voice, to facilitate laryngeal healing.
- To support laryngeal tissue healing, such as hydration, humidification, and avoidance of irritants or allergens, to expedite recovery and prevent recurrence.
Patient Isolation
- Implement droplet precautions for individuals with infectious laryngitis to prevent the transmission of respiratory pathogens.
- Ensure proper signage indicating isolation precautions outside the patient’s room to alert staff and visitors.
- Educate the patient and caregivers on the importance of hand hygiene and respiratory etiquette to reduce the spread of infection.
- Limit unnecessary contact with other patients and healthcare staff to minimize the risk of transmission within healthcare facilities.
- Rationale: Patient isolation is very important to take note of as a nurse to prevent the spread of infectious laryngitis to other patients and healthcare workers. Droplet precautions help contain respiratory droplets, reducing the risk of transmission through coughing or sneezing.
Infection Prevention
- Make sure of the availability of hand hygiene stations and encourage regular handwashing among patients, caregivers, and healthcare staff.
- Give education on proper cough etiquette, including covering the mouth and nose with a tissue or elbow when coughing or sneezing.
- Regularly disinfect high-touch surfaces and equipment in patient rooms and common areas to reduce the risk of environmental contamination.
- Screen visitors and staff for symptoms of respiratory illness and restrict visitation for individuals with symptoms suggestive of infectious laryngitis.
- Rationale: Infection prevention measures, including hand hygiene, respiratory etiquette as a nurse, and environmental cleaning, are essential to minimize the spread of infectious laryngitis within healthcare settings and the community.
Environment
- Maintain a clean and well-ventilated environment on the ward to reduce exposure to environmental irritants that may exacerbate laryngitis symptoms.
- Ensure adequate humidity levels in patient rooms using humidifiers or vaporizers to soothe inflamed throat tissues.
- Minimize noise levels and provide a calm and quiet environment to promote vocal rest and recovery.
- Educate patients and caregivers on environmental modifications to avoid exposure to tobacco smoke, strong odors, and other irritants that can worsen laryngitis symptoms.
- Rationale: Creating a supportive environment with minimal exposure to irritants helps alleviate symptoms and promotes optimal healing and recovery in individuals with laryngitis.
Observation
- Monitor the patient’s respiratory rate, effort, and oxygen saturation to assess respiratory status and detect signs of respiratory distress.
- Assess the patient’s voice quality, pitch, and volume to evaluate changes in vocal function and monitor for improvement or deterioration.
- Monitor for any signs of dehydration, such as dry mucous membranes and decreased urine output, and encourage fluid intake as needed.
- Regularly assess for complications such as worsening hoarseness, persistent fever, or difficulty breathing, and intervene promptly as necessary.
- Rationale: Regular observation and assessment allow for early detection of complications and responses to changes in the patient’s condition, facilitating timely intervention and appropriate care.
Psychological Care
- Give emotional support and reassurance to the patient experiencing distress or frustration due to voice changes and communication difficulties.
- Offer active listening and validation of the patient’s feelings and concerns regarding their condition to address their emotional needs.
- Educate patients and caregivers on coping strategies and communication techniques to manage the psychosocial impact of laryngitis.
- Collaborate with psychologists or social workers to provide counseling or therapy for individuals experiencing significant psychological distress.
- Rationale: Psychological care is essential to address the emotional impact of laryngitis and promote coping strategies to enhance overall well-being and quality of life.
Hygiene
- Encourage frequent hydration to maintain adequate moisture in the throat and prevent dehydration, which can exacerbate laryngitis symptoms.
- Educate a patient on avoiding irritants such as tobacco smoke, strong odors, and alcohol, which can aggravate laryngeal inflammation.
- Recommend throat lozenges or gargling with saltwater to soothe throat irritation and reduce discomfort.
- Educate the patient on proper vocal hygiene practices, including avoiding excessive talking, whispering, or clearing the throat, which can strain the vocal cords.
- Rationale: Hygiene interventions promote throat comfort, reduce irritation, and support vocal recovery in individuals with laryngitis, contributing to symptom relief and overall well-being.
Exercises
- Teach relaxation and breathing exercises to reduce tension in the laryngeal muscles and promote vocal relaxation, aiding in vocal recovery and reducing strain.
- Demonstrate vocal exercises, such as humming, lip trills, or gentle phonation, to improve vocal cord function and reduce vocal strain.
- Encourage regular rest breaks and vocal rest periods to prevent overuse of the voice and facilitate vocal recovery.
- Refer patients to speech-language pathologists for specialized voice therapy and exercises tailored to their specific needs.
- Rationale: Exercise interventions focus on strengthening laryngeal muscles, improving vocal coordination, and promoting vocal health in individuals with laryngitis, supporting optimal vocal recovery and rehabilitation.
Nutrition
- Assess the patient’s nutritional status and dietary intake to identify any deficiencies or dietary factors that may impact laryngitis symptoms.
- Give and encourage a patient to eat a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to support overall health and immune function.
- Give guidance on avoiding spicy, acidic, or excessively hot foods and beverages that can irritate the throat and exacerbate laryngitis symptoms.
- Offer nutritional supplements or fortified foods as needed to address specific nutritional deficiencies or support healing and recovery.
- Rationale: Nutrition interventions aim to support overall health, immune function, and tissue repair in individuals with laryngitis, promoting optimal healing and symptom relief.
Elimination
- Monitor the patient’s fluid intake and output to assess hydration status and ensure adequate urinary elimination.
- Encourage regular bowel movements through the promotion of a high-fiber diet, adequate fluid intake, and physical activity.
- Assess for any urinary retention or constipation symptoms and intervene promptly with appropriate measures.
- Provide education on the importance of maintaining regular bowel and bladder habits for overall health and well-being during laryngitis recovery.
- Rationale: Elimination interventions focus on maintaining optimal fluid balance and bowel function to support hydration, nutritional status, and overall comfort in individuals with laryngitis, promoting holistic patient care and well-being.
Medicine
- Administer prescribed medications, such as antibiotics for bacterial laryngitis or antivirals for viral laryngitis, as indicated.
- Provide analgesics or throat lozenges to alleviate throat pain and discomfort associated with laryngitis.
- Educate patients on the proper use of medications, including dosage, frequency, and potential side effects.
- Monitor the patient’s response to medication therapy and report any adverse reactions or concerns to the healthcare provider.
- Rationale: Medication interventions aim to treat underlying infections, alleviate symptoms, and promote comfort and healing in individuals with laryngitis, optimizing the effectiveness of treatment and patient outcomes.
Advice at Discharge
- Provide education on vocal rest and strategies to minimize vocal strain, such as avoiding shouting or speaking loudly.
- Advise patients to avoid exposure to environmental irritants, such as smoke or pollution, which can exacerbate laryngitis symptoms.
- Recommend adequate hydration and throat lubrication to soothe inflamed throat tissues and reduce discomfort.
- Encourage patients to seek medical attention if symptoms worsen or persist despite self-care measures to prevent complications or progression of the condition.
- Rationale: Providing advice at a disadvantage empowers patients with knowledge and strategies to manage laryngitis symptoms and minimize exacerbating factors, promoting optimal recovery and the prevention of complications.
Prevention of Laryngitis
Hygiene Practices
- Practicing good hygiene, including regular handwashing with soap and water, can help reduce the risk of contracting respiratory infections that can lead to laryngitis.
- Avoiding close contact with individuals who are sick and refraining from sharing personal items such as utensils and drinking glasses can also prevent the spread of infectious agents.
Vocal Hygiene
- Maintaining proper vocal hygiene is essential for preventing vocal strain and laryngeal irritation.
- This includes avoiding yelling or shouting, using amplification devices when speaking in loud environments, and staying hydrated to keep the vocal cords lubricated.
Avoiding Irritants
- Limiting exposure to irritants such as cigarette smoke, air pollution, and chemical fumes can help prevent laryngeal irritation and inflammation.
- Individuals should also be cautious when using their voice in environments with high levels of airborne irritants.
Smoking Cessation
- Quitting smoking is one of the most effective ways to prevent laryngitis and other respiratory conditions.
- Tobacco smoke is a major irritant to the larynx and can increase the risk of developing chronic laryngitis, vocal cord polyps, and laryngeal cancer.
Voice Rest and Vocal Protection
- Taking breaks from talking and resting the voice when experiencing hoarseness or vocal fatigue can prevent overuse and strain of the vocal cords.
- Using amplification devices, such as microphones, can also help reduce vocal strain in situations where speaking loudly is necessary.
Maintaining optimal health
- Strengthening the immune system through regular exercise, balanced nutrition, adequate sleep, and stress management can help reduce the risk of contracting respiratory infections that can lead to laryngitis.
- Avoiding excessive alcohol consumption and staying hydrated can also support overall vocal health.
Allergen Avoidance
- Individuals with known allergies should take steps to avoid exposure to allergens that can trigger allergic laryngitis.
- This may include using air purifiers, keeping windows closed during high pollen seasons, and minimizing contact with animals or other allergenic substances.
Proper Vocal Technique
- Individuals who use their voice professionally, such as singers, actors, and public speakers, should receive training on proper vocal technique to prevent vocal strain and injury.
- This may include working with voice coaches or speech-language pathologists to learn proper breathing, vocal projection, and articulation techniques.
Regular medical check-ups:
- Regular visits to a healthcare provider for preventive care and screenings can help identify and address underlying health conditions that may predispose individuals to laryngitis.
- This includes managing conditions such as gastroesophageal reflux disease (GERD), allergies, and respiratory infections.
Vaccinations
- Staying up-to-date on recommended vaccinations, such as the flu vaccine and pneumococcal vaccine, can help prevent respiratory infections that can lead to laryngitis.
- Vaccinating against common viral infections reduces the risk of developing viral laryngitis and its complications.
Complications
Laryngeal Edema Leading to Airway Obstruction
- Severe inflammation of the larynx can result in laryngeal edema, causing narrowing or complete obstruction of the airway.
- This can lead to respiratory distress and necessitate emergency interventions such as endotracheal intubation or tracheotomy to secure the airway and ensure adequate ventilation.
Sepsis
- In cases of bacterial laryngitis, untreated or inadequately managed infections can lead to the systemic spread of bacteria and subsequent sepsis.
- Sepsis is a life-threatening condition characterized by an overwhelming immune response to infection, resulting in organ dysfunction and tissue damage if not promptly treated with antibiotics and supportive care.
Meningitis
- Rarely, severe bacterial laryngitis can lead to the spread of infection to the meninges, the protective membranes covering the brain and spinal cord, resulting in meningitis.
- Meningitis is a serious condition that requires urgent medical attention and treatment with antibiotics to prevent neurological complications and potential long-term sequelae.
Peritonsillar Abscess
- Laryngitis caused by bacterial infection, particularly group A Streptococcus, can sometimes progress to the development of a peritonsillar abscess.
- This occurs when pus accumulates in the tissues surrounding the tonsils, leading to severe throat pain, difficulty swallowing, and potential complications such as difficulty breathing or aspiration if the abscess ruptures.
Otitis Media
- Inflammatory processes involving the upper respiratory tract, including laryngitis, can predispose individuals to secondary infections such as otitis media, an infection of the middle ear.
- Bacterial or viral pathogens can ascend from the nasopharynx through the Eustachian tube, causing inflammation and fluid accumulation in the middle ear cavity, resulting in ear pain, hearing loss, and potential complications such as tympanic membrane perforation if left untreated.
Pneumonia
- Severe laryngitis, particularly when associated with the aspiration of infected secretions or compromised airway protection, can predispose individuals to the development of pneumonia.
- Pneumonia is characterized by inflammation of the lung tissue and can lead to respiratory failure, sepsis, and other serious complications, especially in vulnerable populations such as the elderly or immunocompromised individuals.
Chronic Laryngitis and Voice Disorders
- Recurrent or persistent laryngitis, especially if left untreated or inadequately managed, can lead to chronic inflammation and structural changes in the larynx, resulting in voice disorders such as chronic hoarseness, vocal fatigue, or vocal nodules.
- These conditions may require long-term management by speech-language pathologists and otolaryngologists to optimize vocal function and quality of life.
Psychosocial Impact
- Chronic or severe laryngitis can have a significant psychosocial impact on individuals, affecting their ability to communicate effectively, participate in social activities, and perform daily tasks.
- Voice changes, pain, and discomfort associated with laryngitis can lead to feelings of frustration, isolation, and impaired quality of life if not adequately addressed through supportive care and rehabilitation interventions.
Read more: Medical-Surgical Nursing
Read more: Hay fever | Causes | Signs and Symptoms | Pathophysiology | Treatment | Nursing Management








[…] Read more: Laryngitis | Causes | Signs and Symptoms | Pathophysiology | Treatment | Nursing Management […]