Ectopic Pregnancy Line Progression
An early pregnancy test line can spark hope, worry, or confusion especially when line darkness changes from day to day. In clinical settings, one frequent question centers on ectopic pregnancy line progression. Do lighter or non-progressing lines signal an ectopic? Can darker lines guarantee a safe intrauterine pregnancy? This comprehensive, evidence-based guide translates hCG physiology and diagnostic pathways into clear, practical insights for nurses, midwives, and clinicians who support patients through uncertain early pregnancy phases.
Ectopic pregnancy remains a time-sensitive condition, and while home pregnancy test lines can offer clues, line progression alone cannot diagnose location or viability. Understanding what line changes can and cannotreveal is essential to promote safe, timely assessment and care.
Defining Ectopic Pregnancy and Why Early Signals Matter
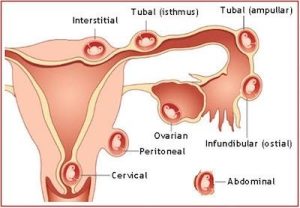
Ectopic pregnancy occurs when a fertilized egg implants outside the uterine cavity, most commonly in the fallopian tube (ampullary region), but also potentially in the isthmus, fimbria, interstitium, cervix, ovary, or peritoneal cavity. Without early recognition and intervention, rupture can lead to life-threatening internal hemorrhage.
Key epidemiology and impact:
- Incidence: Approximately 1–2% of all reported pregnancies.
- Morbidity: Leading cause of first-trimester maternal mortality in many regions.
- Recurrence risk: Higher in patients with a history of ectopic pregnancy.
Risk factors to flag during assessment:
- Prior ectopic pregnancy
- Tubal surgery, pelvic or abdominal surgery with adhesions
- History of pelvic inflammatory disease or chlamydia/gonorrhea
- Current intrauterine device (IUD) in place at conception
- Assisted reproductive technologies (e.g., IVF), ovulation induction
- Endometriosis
- Tobacco use
- Increasing maternal age
Clinical presentations range from asymptomatic early detection to acute abdomen with hemodynamic instability. Asymmetry between symptoms and test results is common; hence a structured approach to testing and trending beta-hCG levels is essential.
What “Line Progression” Means in Home Pregnancy Tests
“Line progression” refers to the perceived darkening of the test line on serial qualitative home urine tests. Many users compare test line intensity day by day, expecting darker lines as pregnancy advances.
How home tests work:
- Home pregnancy tests detect human chorionic gonadotropin (hCG) in urine.
- Most over-the-counter (OTC) tests detect total hCG at thresholds ranging from ~10 to 25 mIU/mL.
- Positive tests occur when hCG concentration exceeds the assay’s sensitivity threshold.
- Line intensity can correlate loosely with concentration—within a narrow range and with high variability.
Important caveats:
- Urine concentration varies: hydration status, time of day, and duration since last void influence hCG concentration.
- Brand and batch differences: assay chemistry, line dye, and sensitivity differ among products and lots.
- Saturation and “dye stealer” phenomena: extremely high hCG can cause the control line to appear lighter than the test line, confounding interpretation.
- Evaporation lines: faint, colorless lines appearing after the recommended read time can be misinterpreted as positives.
- Subjective perception: lighting, camera exposure, and display screens alter perceived line intensity.
Bottom line for clinical decision-making: qualitative line progression is not a reliable diagnostic modality for pregnancy location or viability. Quantitative serum hCG and transvaginal ultrasound (TVUS) remain the standards for evaluating ectopic pregnancy risk and early pregnancy outcomes.
hCG Physiology and Its Relationship to Line Appearance
hCG is produced by trophoblastic tissue after implantation. Circulating hCG supports the corpus luteum, stabilizes progesterone production, and signals early placental development.
Expected hCG dynamics:
- Viable intrauterine pregnancy (IUP): the slowest acceptable rise over 48 hours is approximately 35% (updated evidence), not necessarily a doubling every 48 hours. Many viable pregnancies double every 48–72 hours, but ranges vary significantly, especially as baseline values increase.
- Early pregnancy loss: typical pattern is a falling hCG, often with a predictable half-life, though decline rates vary.
- Ectopic pregnancy: hCG often rises more slowly than in a viable IUP, plateaus, or fluctuates with small increases or decreases.
Serum vs urine:
- Serum hCG (quantitative) offers precise values and enables calculation of rise or fall over time.
- Urine hCG correlates with serum levels but shows wider variability due to dilution, timing, and assay differences.
- Consequently, urine-based line progression lacks the clinical precision required to guide ectopic pregnancy decisions.
Ectopic Pregnancy Line Progression Patterns: What To Recognize
While line progression cannot diagnose ectopic pregnancy, certain qualitative patterns may coincide with ectopic risk when considered alongside symptoms and quantitative data.
Common patterns seen in practice:
- Persistently faint positive lines over multiple days: may indicate low or slowly rising hCG, compatible with very early IUP, early pregnancy loss, or ectopic pregnancy. Not diagnostic without serum testing and ultrasound.
- Lines that darken initially then plateau: may coincide with a plateau or minimal rise in serum hCG; requires serial trending and imaging.
- Lines that lighten after initial dark positives: can occur with biochemical pregnancy or evolving early loss; ectopic pregnancy remains on the differential until ruled out.
- “Dye stealer” presentation: a very dark test line compared with the control can occur with high hCG but does not guarantee uterine location.
Clinical note: symptoms such as unilateral pelvic pain, shoulder tip pain, syncope, or heavy vaginal bleeding demand urgent evaluation regardless of line appearance.
Diagnostic Approach When Ectopic Pregnancy Is Suspected
A structured, evidence-based pathway ensures timely detection and safe management.
Initial Clinical Assessment
- Focused history: last menstrual period (LMP), conception attempts, fertility treatments, prior ectopic, prior pelvic/tubal surgery, pelvic infections, IUD presence at conception, smoking, prior early losses.
- Symptom review: lower abdominal/pelvic pain (often lateralized), vaginal spotting or bleeding, dizziness/syncope, shoulder tip pain, gastrointestinal upset.
- Physical exam: vital signs, abdominal/pelvic tenderness, peritoneal signs, cervical motion tenderness (CMT), adnexal mass or fullness if palpable.
- Immediate red flags: hypotension, tachycardia, severe abdominal pain, peritoneal signs prioritize emergent imaging and surgical evaluation.
Laboratory Evaluation
- Quantitative serum hCG: obtain baseline and repeat at approximately 48-hour intervals. Interpret change (rise or fall) rather than a single value.
- CBC: assess hemoglobin/hematocrit for bleeding, white count (nonspecific).
- Blood type and Rh factor: if RhD-negative and bleeding or miscarriage concern, plan Rh(D) immune globulin administration per protocol.
- Serum progesterone (optional): low values may support nonviability but cannot localize pregnancy.
Transvaginal Ultrasound and the Discriminatory Zone
- TVUS is the imaging modality of choice in early pregnancy.
- Discriminatory zone: the serum hCG level above which an intrauterine gestational sac is typically visible by TVUS. Commonly cited range: 1,500–3,500 mIU/mL (lab and operator dependent).
- Cautions:
- Absence of an intrauterine sac above the discriminatory zone increases suspicion for ectopic pregnancy but is not solely diagnostic.
- A single hCG measurement should not determine management. Serial values and repeat imaging are often necessary.
- A yolk sac or fetal pole within the uterus confirms intrauterine location; a pseudosac can mimic an early sac in ectopic pregnancy, making experienced sonography critical.
Serial hCG Ratios and Clinical Interpretation
- Calculate the 48-hour hCG ratio: hCG48 / hCG0.
- Viable IUP often shows ratio ≥1.35 (≥35% rise), but some viable pregnancies rise more slowly.
- Ectopic pregnancy commonly shows smaller rises (<35%), plateaus, or minimal declines.
- Early loss often shows a declining pattern.
- Pregnancy of Unknown Location (PUL):
- Positive hCG with no definitive intrauterine or extrauterine pregnancy on TVUS.
- Manage with close follow-up, serial hCG, and repeat ultrasound until diagnosis declares: viable IUP, early loss, or ectopic.
Urine Testing Pitfalls and the Hook Effect
- High-dose hook effect: very high hCG can overwhelm some immunoassays, paradoxically leading to weak or negative lines. Rare in very early pregnancy; more common later or with trophoblastic disease.
- Test variability: inter-brand differences and user technique affect line intensity.
- Clinical takeaway: qualitative urine testing serves as a screening tool; management decisions require serum hCG and imaging.
Why Ectopic Pregnancy Line Progression Is Not Diagnostic
- Pregnancy test lines are qualitative or semi-quantitative at best; small day-to-day differences in urine concentration overshadow modest changes in circulating hCG.
- Many ectopic pregnancies initially present with standard or even robust urine positives; conversely, many non-ectopic pregnancies show slow line changes yet remain viable.
- Diagnostic certainty relies on integrated data: symptoms, serial quantitative hCG, and high-quality transvaginal ultrasound, with vigilant follow-up.
Management Options for Ectopic Pregnancy
Management prioritizes hemodynamic stability, resolution of trophoblastic tissue, pain control, and fertility preservation when possible. Choice depends on clinical stability, hCG level and trajectory, imaging findings, patient preferences, and access to reliable follow-up.
Expectant Management (Selected Cases)
- Criteria (typical): hemodynamically stable, minimal symptoms, low and consistently declining hCG, no sign of rupture, reliable access to follow-up, small adnexal mass (if present) without fetal cardiac activity.
- Monitoring: serial hCG until non-pregnant levels; counsel on emergency symptoms; establish 24/7 access to care.
- Success rates: higher with initial low hCG and clear downward trend.
Medical Management With Methotrexate
- Indications: hemodynamically stable, confirmed or high-suspicion ectopic, no contraindications, no evidence of rupture, and appropriate follow-up feasibility.
- Common protocol: single-dose methotrexate 50 mg/m² intramuscular on day 1, with hCG checks on day 4 and day 7. Expect ≥15% decline from day 4 to day 7. If decline <15%, consider a second dose or surgery.
- Alternative regimens: two-dose or multi-dose protocols in select cases.
- Typical candidate profile:
- No fetal cardiac activity on ultrasound
- Adnexal mass size usually less than 3.5–4 cm (varies by guideline)
- Baseline hCG at lower to moderate range (success declines with higher hCG)
- Contraindications:
- Hemodynamic instability or suspected rupture
- Renal, hepatic, or hematologic dysfunction; peptic ulcer disease
- Active pulmonary disease
- Immunodeficiency
- Sensitivity to methotrexate
- Inability to ensure close follow-up
- Counseling points during MTX therapy:
- Avoid folic acid supplements and high-folate foods that may negate MTX activity (institutional protocols vary; registered dietitian guidance may help).
- Avoid NSAIDs if contraindicated per protocol.
- Refrain from vigorous physical activity and intercourse until resolution due to rupture risk.
- Minimize sun exposure to reduce photosensitivity.
- Confirm contraception planning until hCG resolves; conception timing after MTX often delayed for at least one menstrual cycle up to three months depending on counseling practices.
Surgical Management
- Indications:
- Hemodynamic instability
- Suspected rupture
- Contraindication or failure of methotrexate
- High hCG levels with significant symptoms or large adnexal mass
- Patient preference for definitive treatment
- Procedures:
- Laparoscopic salpingostomy: preserves the tube by removing trophoblastic tissue; requires diligent follow-up for persistent trophoblast.
- Laparoscopic salpingectomy: removal of the affected tube; offers definitive treatment with lower risk of persistent trophoblast.
- Other sites (interstitial, cervical, cesarean scar, ovarian, abdominal) may require specialized approaches, sometimes combined with interventional radiology or adjunctive methotrexate.
Post-Treatment Monitoring and Follow-Up
- Serial hCG to non-pregnant levels confirms resolution.
- Persistent trophoblast: if hCG plateaus or rises post-salpingostomy or after MTX, consider additional MTX or surgical intervention.
- RhD-negative patients with bleeding typically receive Rh(D) immune globulin per guidelines.
Nursing Responsibilities: Assessment, Safety, Education, and Advocacy
Nurses are pivotal in early recognition and ongoing care for suspected ectopic pregnancy.
Assessment and Triage:
- Rapid identification of red flags: hypotension, tachycardia, severe abdominal pain, syncope, shoulder tip pain.
- Focused history on risk factors and timing of symptoms.
- Pain assessment using validated scales; document onset, quality, location, and progression.
- Estimate bleeding: pad counts, clots, associated symptoms (dizziness, fatigue).
Diagnostics and Coordination:
- Prompt venipuncture for quantitative hCG, CBC, and type and screen.
- Arrange urgent TVUS with clear communication of suspicion level to imaging teams.
- Establish reliable follow-up scheduling for repeat hCG and ultrasound, particularly for PUL cases.
Medication Management:
- Verify methotrexate dosing (BSA-based) and contraindications.
- Administer MTX per protocol, counsel on precautions, and schedule day 4 and day 7 hCG checks.
- Monitor for side effects such as nausea, stomatitis, and photosensitivity. Escalate care for abdominal pain that may signify rupture versus expected “separation pain.”
Patient-Centered Counseling:
- Explain that pregnancy test line progression cannot localize a pregnancy and should not guide safety decisions.
- Reinforce the need for serial hCG and imaging until diagnosis is clear.
- Provide clear return precautions: increasing pain, heavy bleeding, dizziness or fainting, shoulder tip pain, or any new concerning symptoms—emergent evaluation indicated.
Documentation:
- Record all counseling, results, hCG values with dates/times, imaging impressions, and management plans.
- Ensure accurate contact information and contingency plans if follow-up is missed.
- Document Rh status and Rh(D) immune globulin administration when indicated.
Interprofessional Collaboration:
- Engage early with obstetrics/gynecology, emergency medicine, radiology, and, if needed, interventional radiology.
- Case review for complex or atypical presentations (heterotopic pregnancy, cesarean scar ectopic, interstitial ectopic).
Psychosocial Support:
- Acknowledge uncertainty and emotional burden that often accompany early pregnancy complications.
- Offer resources for mental health support, bereavement, or fertility counseling if requested.
- Consider cultural, linguistic, and health literacy needs in all communications.
Clinical Scenarios Illustrating Ectopic Pregnancy Line Progression Pitfalls
Scenario 1: Persistent Faint Lines, Mild Cramping
A patient presents with five days of faint positive home tests after a missed period, reporting mild unilateral cramping. Serum hCG is 120 mIU/mL; 48 hours later, 145 mIU/mL (21% rise). TVUS shows no intrauterine sac, consistent with PUL. The slower-than-expected hCG rise raises concern for ectopic pregnancy. Repeat hCG at 96 hours continues to show a minimal increase. After informed decision-making, medical management with methotrexate is initiated. Home line progression did not provide diagnostic clarity; quantitative measures guided safe care.
Scenario 2: Darkening Lines, New Shoulder Tip Pain
A patient reports progressively darker lines over a week and now has severe abdominal pain with shoulder tip pain. Vital signs show tachycardia and borderline hypotension. Serum hCG is 2,800 mIU/mL. TVUS shows no intrauterine pregnancy and free fluid in the pelvis. Emergent surgical intervention confirms a ruptured tubal ectopic. Despite “strong” line progression, the pregnancy was extrauterine.
Scenario 3: Dye Stealer With Early Bleeding
A patient demonstrates a “dye stealer” on an early home test and light spotting. Quantitative hCG is 7,500 mIU/mL; TVUS confirms an intrauterine gestational sac with yolk sac. The dark line reflected high hCG but, alone, would not have ruled out ectopic pregnancy without imaging.
Takeaway: Home line patterns can mislead. Safety rests on a protocolized combination of symptoms, serial hCG, and ultrasound.
Myth vs Fact: Ectopic Pregnancy Line Progression
- Myth: Darker lines rule out ectopic pregnancy.
- Fact: A strong or dark line only indicates hCG presence, not pregnancy location.
- Myth: Faint, non-progressing lines automatically indicate ectopic pregnancy.
- Fact: Many early intrauterine pregnancies and biochemical pregnancies produce faint or slowly changing lines. Ectopic pregnancy is one possibility among several.
- Myth: A single high hCG value proves a healthy pregnancy.
- Fact: A single value lacks context. Location and viability require trend analysis and imaging.
- Myth: The discriminatory zone guarantees a visible intrauterine sac at a specific hCG value.
- Fact: Operator expertise, equipment, and individual variation affect visualization. Repeat imaging and trending are key.
Special Situations
Pregnancy of Unknown Location (PUL):
- Management requires close follow-up and diagnostics until a definitive location is identified or hCG resolves.
- Risk of ectopic persists until proven otherwise.
Heterotopic Pregnancy:
- Coexistence of intrauterine and ectopic pregnancies. More common with assisted reproduction.
- Presence of an intrauterine pregnancy does not eliminate ectopic risk; persistent pain or atypical findings prompt continued evaluation.
Interstitial and Cesarean Scar Ectopics:
- Unique risks include later rupture and heavier bleeding.
- Ultrasound findings may be subtle; 3D ultrasound or MRI and specialist consultation may be needed.
RhD Considerations:
- RhD-negative patients with first-trimester bleeding generally receive Rh(D) immune globulin per institutional protocols.
H2: Practical Algorithm for Suspected Ectopic Pregnancy
- Assess stability
- Unstable: initiate resuscitation, urgent OB/GYN consult, and prompt operative evaluation.
- Order baseline labs and TVUS
- Quantitative hCG, CBC, type and screen (and crossmatch if needed).
- TVUS to evaluate for intrauterine or extrauterine pregnancy, adnexal mass, and free fluid.
- Interpret results in context
- IUP identified: manage per early pregnancy guidelines.
- Ectopic visualized: consider MTX vs surgery based on stability, size, cardiac activity, and preferences.
- PUL: repeat hCG in ~48 hours and repeat TVUS as indicated.
- Follow serial hCG
- Rising ≥35% in 48 hours: favors viable IUP but not guaranteed; continue ultrasound follow-up if no sac visible.
- Plateau or sub-threshold rise: raises ectopic risk; consider MTX or further imaging per protocol.
- Falling hCG: likely early loss; monitor to resolution. Ectopic still possible until hCG reaches zero and clinical status remains stable.
- Provide safety netting and support
- Clear return precautions, scheduled follow-up, and counseling resources.
Education Points to Share With Patients and Families
- Home pregnancy tests confirm hCG presence, not pregnancy location.
- “Line progression” is not a diagnostic tool for ectopic pregnancy.
- Serial quantitative hCG and transvaginal ultrasound are essential for early pregnancy assessment.
- Urgent care is needed for severe abdominal pain, heavy bleeding, syncope, or shoulder tip pain.
Quality and Safety Considerations for Nursing Teams
- Protocol adherence: standardized ectopic pregnancy pathways reduce delays and improve outcomes.
- Diagnostic stewardship: avoid overreliance on single hCG values or urine line impressions; prioritize integrated interpretation.
- Communication clarity: ensure consistent messages across teams to prevent confusion during follow-up.
- Equity and access: address barriers to timely imaging and repeat labs; facilitate transportation and interpreter services when needed.
- Documentation excellence: precise, time-stamped recording of hCG values and imaging enhances continuity and safety.
Frequently Asked Questions (FAQ)
Can ectopic pregnancy cause a positive pregnancy test with strong line progression?
Yes. Ectopic pregnancies commonly produce hCG, which can create strong test lines. Line strength alone cannot determine pregnancy location or safety.
Do faint lines over several days mean ectopic pregnancy?
Not necessarily. Persistent faint lines can occur with very early intrauterine pregnancy, biochemical pregnancy, or ectopic pregnancy. Serial serum hCG and ultrasound determine the diagnosis.
What is the discriminatory zone, and how is it used?
The discriminatory zone is an hCG range (commonly 1,500–3,500 mIU/mL) above which a gestational sac is typically visible in the uterus on transvaginal ultrasound. Absence of an intrauterine sac above this level raises ectopic concern but is not definitive without further evaluation.
How fast should hCG rise in a viable pregnancy?
In early viable intrauterine pregnancies, a minimal increase of about 35% over 48 hours is generally acceptable. Many pregnancies rise faster, but trends must be interpreted with ultrasound findings.
When is methotrexate used for ectopic pregnancy?
Methotrexate is used for stable patients with confirmed or highly suspected ectopic pregnancy who meet eligibility criteria and have no contraindications. Close hCG monitoring ensures treatment success.
Conclusion
Ectopic Pregnancy Line Progression is a popular topic in online forums and early pregnancy conversations, but it is not a diagnostic tool. Clinical safety depends on integrating history, symptoms, serial quantitative hCG trends, and high-quality transvaginal ultrasound. Nurses play a central role in rapid recognition, evidence-based counseling, meticulous follow-up, and compassionate support. By following standardized pathways and prioritizing patient safety over home line interpretations, care teams improve outcomes and reinforce trust during a vulnerable period of early pregnancy.
References and Evidence Base (selected for context)
- Barnhart KT. Clinical practice. Ectopic pregnancy. N Engl J Med. 2009;361(4):379–387.
- Morse CB, Sammel MD, Shaunik A, et al. Performance of human chorionic gonadotropin curves in women at risk for ectopic pregnancy. Obstet Gynecol. 2012.
- Doubilet PM, Benson CB, Bourne T, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013.
- American College of Obstetricians and Gynecologists (ACOG). Practice Bulletin: Tubal Ectopic Pregnancy.
- Society of Radiologists in Ultrasound (SRU). Consensus statement on early first-trimester ultrasound.
- Royal College of Obstetricians and Gynaecologists (RCOG). The Management of Early Pregnancy Loss and Ectopic Pregnancy.
Note: This article is for professional education. Clinical decisions should follow local protocols, current guidelines, and specialist consultation when needed.