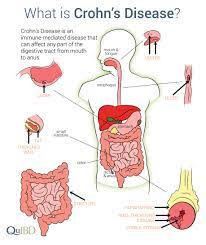
Crohn’s disease is a chronic inflammatory condition of the gastrointestinal system, primarily impacting the distal ileum and colon. However, it can also affect any part of the digestive tract, from the mouth to the anus. This disorder is characterized by nonspecific inflammation, and its exact cause remains unknown. Crohn’s disease manifests as an idiopathic inflammatory process that can involve any segment of the gastrointestinal tract.
Epidemiology
Crohn’s disease can develop at any age, but it most commonly occurs between 25 and 30 years old. Both men and women are affected, with a slightly higher incidence among women. One-third of cases primarily involve the small bowel, often affecting the terminal ileum (ileitis). Approximately half of cases involve both the small bowel and colon, with the terminal ileum and adjacent proximal ascending colon being most commonly affected (ileocolitis). In 15-20% of cases, only the colon is affected.
Management
Aims
- Control the inflammatory process.
- Relieve symptoms.
- Correct metabolic and nutritional problems and promote healing.
Diagnostic Studies
- Proctosigmoidoscopy: is typically the initial procedure to assess inflammation in the rectosigmoid area.
- Stool Occult Blood Test.
- Barium Enema: useful for identifying strictures and fissures.
- Small Bowel X-ray: Can reveal irregular mucosa, ulcerations, and stiffening.
- Sigmoidoscopy and colononoscopy: These procedures show patchy areas of inflammation.
- Biopsy: Obtained during sigmoidoscopy, it reveals granulomatous tissue.
- Blood tests: These may demonstrate an increased white blood cell count, a reduced erythrocyte sedimentation rate (ESR), and a decreased hemoglobin level.
Drug Therapy
While there is no specific therapy for Crohn’s disease, the following drugs may help manage symptoms:
- Corticosteroids (e.g., Prednisolone):
- Dosage: Prednisolone 5–60 mg daily orally, given as a single dose or in divided doses. The maximum daily dose is 250mg.
- Mode of Action: stimulates the synthesis of enzymes to decrease the inflammatory response.
- Side Effects: suppression of the immune system, resulting in lymphocytopenia.
- Aminosalicylates (e.g., Sulfasalazine):
- Dosage: Initial 3–4 g orally daily in divided doses, followed by a maintenance dose of 2g orally daily in divided doses.
- Mode of Action: Believed to be metabolized by intestinal flora in the colon, producing anti-inflammatory and antibacterial effects.
- Side Effects: reduced appetite, stomatitis, vertigo.
- Antibiotics (e.g., Metronidazole):
- Dosage: 200–400 mg orally three times daily for 7–10 days.
- Mode of Action: Bactericidal action by inhibiting bacterial DNA synthesis.
- Side Effects: dry mucous membranes, metallic taste.
- Anti-Diarrheals (e.g., Loperamide):
- Dosage: 4mg initially orally, then 2mg per loose stool. The maximum dose is 16mg in 24 hours.
- Mode of Action: Reduces intestinal motility and fluid secretion.
- Side Effects: constipation, abdominal pain, dry mouth, drowsiness.
- Analgesics (e.g., Paracetamol):
- Dosage: 500–1000 mg orally three times daily.
- Mode of Action: non-narcotic analgesic, antipyretic, and anti-inflammatory.
- Side Effects: Rare, but may include nausea, vomiting, and liver damage.
Read more: Medical-Surgical Nursing
Read more: Malabsorption Syndrome | Etiology, Nursing Care Management



[…] Read more: Crohn’s Disease | Causes | Pathophysiology | Nursing Management […]