What is bronchitis?
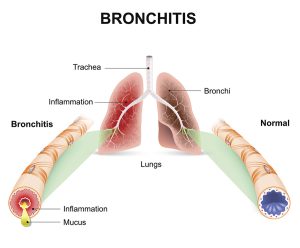
Overall, bronchitis affects the respiratory system, particularly the bronchial tubes, and manifests with symptoms such as coughing and breathing difficulties.
Causes of Bronchitis
- Microorganisms: Bronchitis can be triggered by various microorganisms, including viruses and bacteria. These pathogens infiltrate the bronchial tubes, leading to inflammation and respiratory distress.
- Extension of Infection from the Trachea: Infections originating in the trachea can extend downward into the bronchial passages, exacerbating inflammation and disrupting normal respiratory function.
- Traumatic Injuries: Traumatic injuries to the chest area can disrupt the integrity of the respiratory system, potentially leading to inflammation of the bronchial tubes and subsequent bronchitis.
- Excessive Cold Air: Exposure to excessively cold air can irritate the bronchial tubes, making individuals more susceptible to bronchitis by compromising the respiratory tract’s natural defenses.
- Smoking: Smoking is a significant risk factor for bronchitis, as the chemicals in tobacco smoke damage the bronchial lining, weaken the immune response, and contribute to chronic inflammation of the airways.
- Overexposure to Industrial Fumes: Workers exposed to industrial fumes, such as those found in manufacturing or chemical processing environments, are at risk of developing bronchitis due to respiratory irritation and inflammation caused by these harmful substances.
Types
There are 2 types of bronchitis, and these are:
- Acute bronchitis
- Chronic bronchitis
Acute bronchitis
Acute bronchitis refers to inflammation of the bronchial tree with minimal structural alterations in the affected areas. It typically presents with symptoms such as coughing or a slight irritation in the throat, sometimes accompanied by the production of sputum.
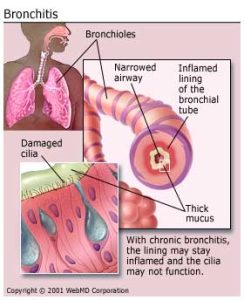
The primary cause of acute bronchitis is viral infections targeting the bronchial epithelium, leading to inflammation and heightened mucus production within the bronchi.
Causes of Acute Bronchitis
Viral Infections: Acute bronchitis is frequently triggered by viral infections, with several types of viruses implicated in its onset. Common viral culprits include rhinoviruses, coronaviruses, adenoviruses, metapneumoviruses, parainfluenza viruses, respiratory syncytial virus (RSV), and influenza viruses.
These viruses infect the epithelial cells lining the bronchial tubes, provoking inflammation and increased mucus production, which contribute to the characteristic symptoms of acute bronchitis.
Bacterial Infections: While less common than viral causes, bacterial infections can also lead to acute bronchitis. Bacteria such as Mycoplasma pneumoniae, Chlamydophila pneumoniae, Bordetella pertussis, and Streptococcus pneumonia are known to provoke bronchial inflammation and respiratory symptoms.
These bacteria may infect the bronchial epithelium, triggering an immune response and causing the characteristic symptoms of acute bronchitis.
Signs and Symptoms of Acute Bronchitis
- Dry Cough Progressing to Productive Cough: Initially, acute bronchitis often presents with a dry cough that may later transition to a productive cough, characterized by the expulsion of mucus or phlegm from the bronchial tubes.
- Chest Pains: Individuals with acute bronchitis may experience discomfort or pain in the chest area, often due to the persistent coughing and inflammation of the bronchial passages.
- Haemoptysis (Coughing up Blood-Stained Sputum): In some cases, acute bronchitis can lead to haemoptysis, where individuals cough up sputum tinged with blood. This symptom warrants prompt medical attention.
- General Body Malaise: Acute bronchitis can cause a feeling of overall body malaise, characterized by fatigue, weakness, and a general sense of discomfort or unease.
- Dyspnoea (Shortness of Breath): Shortness of breath, or dyspnoea, is a common symptom of acute bronchitis, particularly during physical exertion or when breathing becomes more labored due to bronchial inflammation.
- Fatigue: Fatigue is a prevalent symptom accompanying acute bronchitis, as the body expends energy to combat the underlying infection and cope with the respiratory distress.
- Sore Throat: Many individuals with acute bronchitis experience a sore throat, which can result from irritation of the throat tissues due to coughing or from the viral or bacterial infection affecting the upper respiratory tract.
- Cyanosis: In severe cases, cyanosis may occur, characterized by a bluish discoloration of the skin or mucous membranes, indicating a decrease in oxygen saturation in the blood.
- Nasal Congestion: Acute bronchitis may also be accompanied by nasal congestion, as the respiratory infection can extend to the upper airways, leading to inflammation and congestion of the nasal passages.
Chronic bronchitis
History and Physical Examination for Bronchitis:
History
- Symptom Duration and Severity: Ask the patient about the duration and severity of symptoms such as cough, sputum production, dyspnea, chest pain, and fatigue.
- Risk Factors: Ask about patient risk factors such as smoking history, occupational exposures, environmental pollution, and previous respiratory infections.
- Medical History: Ask for any pre-existing conditions such as asthma, allergies, COPD, or immunocompromised status.
- Recent Illnesses: Ask if the patient has had recent upper respiratory infections or exacerbations of chronic respiratory conditions.
- Medication History: Assess for any recent medication use, including antibiotics, bronchodilators, or corticosteroids.
- Functional Impact: Evaluate how symptoms affect daily activities, sleep, and overall quality of life.
Physical Examination
- Vital Signs: Measure vital signs, including temperature, heart rate, respiratory rate, and oxygen saturation.
- Respiratory Examination: Auscultate lung fields for abnormal breath sounds such as wheezes, crackles, or diminished breath sounds. Evaluate respiratory effort and chest expansion.
- Cough Assessment: Observe the character of the cough (dry or productive), and inquire about factors that exacerbate or alleviate coughing.
- Sputum Evaluation: Assess the quantity, color, and consistency of the sputum produced.
- Chest Examination: Palpate the chest for tenderness or deformities. Percuss to assess for dullness or hyper-resonance, indicating possible consolidation or hyperinflation.
- Cardiovascular Examination: Perform a focused cardiovascular examination to evaluate for signs of cardiac involvement or complications.
- General Examination: Assess for signs of systemic illness such as fever, malaise, weight loss, or peripheral edema.
Treatment for Bronchitis
Effective management of bronchitis involves a multifaceted approach aimed at relieving symptoms, reducing inflammation, and addressing the underlying cause:
- Antibiotics: If the bronchitis is caused by a bacterial infection, antibiotics such as ampicillin may be prescribed to target the bacterial pathogens and prevent complications. However, antibiotics are not routinely recommended for viral bronchitis.
- Anti-Inflammatory Drugs: Anti-inflammatory medications like prednisolone may be prescribed to reduce inflammation in the airways, alleviate swelling, and ease breathing difficulties associated with bronchitis.
- Cough expectorants: Cough expectorants such as ammonium chloride may be used to help thin and loosen mucus, making it easier to cough up and expel from the airways. This can help relieve coughs and promote the clearance of respiratory secretions.
- Steam Inhalations: Steam inhalations can help moisten and loosen mucus, making it easier to clear from the airways. Inhaling steam from a bowl of hot water or using a humidifier can provide relief from congestion and soothe irritated airways.
- Environmental Considerations: Creating a warm, well-ventilated room environment can help ease symptoms of bronchitis. Avoiding exposure to cold air, tobacco smoke, and other respiratory irritants can help prevent the exacerbation of symptoms.
- Hydration and Nutrition: Maintaining hydration is important during bronchitis to help thin mucus and prevent dehydration. Drinking plenty of fluids and consuming a light, nutritious diet can support the immune system and aid in recovery.
- Rest and Comfort Measures: Encouraging adequate rest and relaxation can support the body’s healing process during bronchitis. Providing comfort measures such as warm blankets and soothing throat lozenges can help alleviate discomfort and promote recovery.
- Monitoring and Follow-Up: Regular monitoring of symptoms and follow-up with healthcare providers is important to track progress and ensure appropriate management of bronchitis. In severe cases or if symptoms persist or worsen, further medical evaluation may be necessary.
Investigations for Bronchitis
Effective diagnosis of bronchitis involves a comprehensive assessment combining various investigative techniques:
- Chest X-ray: Chest X-rays may reveal hyperinfiltration and increased bronchovascular markings, providing insights into the extent of inflammation and potential complications such as pneumonia or chronic obstructive pulmonary disease (COPD).
- Pulmonary Function Tests (PFTs): Pulmonary function tests, including spirometry, assess lung function parameters such as vital capacity, forced expiratory flow, and residual volume. In bronchitis, PFTs typically demonstrate increased residual volume, decreased vital capacity, and forced expiratory flow, along with normal static compliance and diffusion capacity.
- Arterial Blood Gas (ABG) Analysis: Arterial blood gas analysis provides valuable information about oxygenation and ventilation status. In bronchitis, ABG analysis often reveals decreased arterial oxygen tension (PaO2) due to impaired gas exchange, along with normal or increased arterial carbon dioxide tension (PaCO2), indicating respiratory compensation.
- Sputum Culture: Sputum culture may be performed to identify the presence of microorganisms and assess neutrophil levels, aiding in determining the underlying cause of bronchitis and guiding appropriate antibiotic therapy if bacterial infection is suspected.
- Electrocardiogram (ECG): An electrocardiogram may be conducted to assess cardiac function, particularly in cases where bronchitis coexists with cardiovascular conditions. ECG findings may reveal atrial arrhythmias, which can occur secondary to hypoxemia or as a consequence of chronic lung disease.
Nursing Management
Aims
- To maintain clear airway
- To maintain circulation
- To promote quick recovery
- To prevent complications such as respiratory failure
Read more: Medical-Surgical Nursing
Read more: Asthma | Classifications | Risk Factors | Sign and symptoms | Pathophysiology | Nursing Management



[…] Read more: Bronchitis | Causes | Signs and symptoms | Pathophysiology | Treatment | Nursing Management […]