CDH is a relatively rare but severe birth defect. It occurs in approximately 1 in 2500 to 5000...
Author - Albey BSc N
Nursing Diagnosis for Hypertension
You might be surprised to learn that more than 1. Is it true that 13 Million people across the...
Nursing Diagnosis for Pneumonia
Pneumonia is a leading cause of death and claims more than one million lives in the United States...
Impaired Skin Integrity Nursing Diagnosis
Every year, 2. Pressure injuries result in more than 60 thousand deaths per year; 5 million patient...
Registered Nurse Career Guide: How to Become a Registered Nurse...
There is the fact that about 3 million of nurses are registered in the United States of America. It...
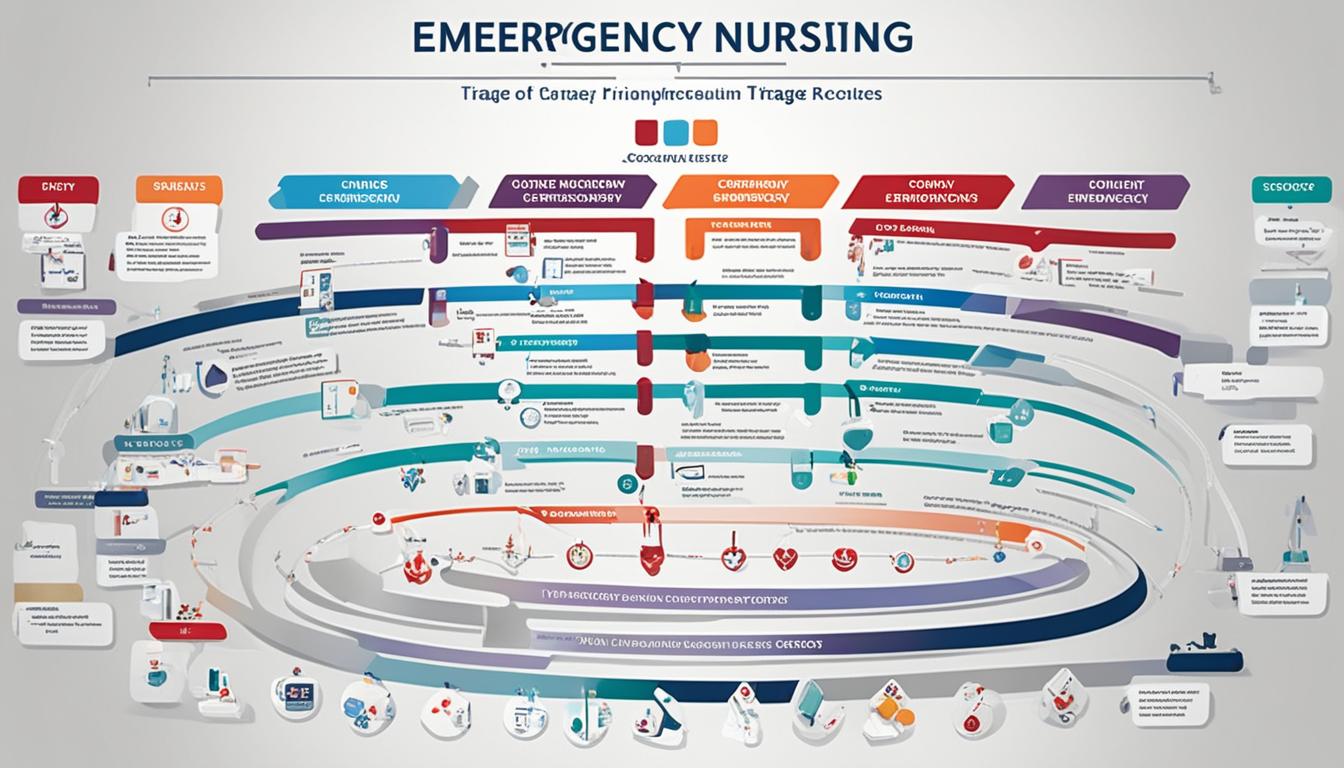
Emergency nursing triage
Especially in the codes of emergency medicine, time is of essence and many actions can mean life...
Adult Gerontology Acute Care Nurse Practitioner
You would not believe it but the employment of Adult Gerontology Acute Care Nurse Practitioners...
NCLEX Practice Questions Test Bank for Free
NCLEX Exam Quiz Guidelines Familiarize Yourself with the Format: The NCLEX exam includes multiple...
Nursing Care Plans (NCP): Ultimate Guide and List
Welcome to our comprehensive guide on nursing care plans (NCP)! Whether you are a nursing student...
Revolutionizing Health: The Care Plan Approach to Nursing
Introduction to the Care Plan Approach From the onset of a nurse’s role in patient care, a...