Mental health, a dynamic and intricate facet of human well-being, encompasses various dimensions that contribute to an individual’s overall psychological state. In this exploration, we delve into the diverse aspects that constitute mental health, shedding light on its complexities and the interconnected factors that influence it.
1. Emotional Well-Being
Understanding Emotions
Emotional well-being is a cornerstone of mental health. It involves recognizing, understanding, and effectively managing a spectrum of emotions, from joy and contentment to sadness and anger. Cultivating emotional intelligence plays a pivotal role in fostering a resilient mental state.
2. Social Connections
The Impact of Social Relationships
Human beings are inherently social creatures, and the quality of social connections significantly influences mental health. Strong, positive relationships contribute to a sense of belonging, support, and fulfillment, while isolation and strained relationships can have adverse effects on mental well-being.
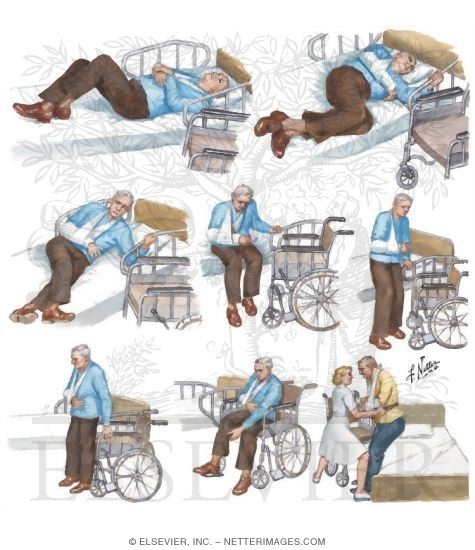
3. Psychological Resilience
Navigating Life’s Challenges
Psychological resilience is the ability to bounce back from adversity and navigate life’s challenges with fortitude. Building resilience involves developing coping mechanisms, adaptability, and a positive mindset, empowering individuals to face setbacks and uncertainties.
4. Cognitive Functioning
The Mind’s Operations
Cognitive functioning encompasses various mental processes, including perception, memory, problem-solving, and decision-making. Mental health relies on the efficient functioning of these cognitive processes, ensuring clarity of thought, effective problem-solving, and the ability to learn and adapt.
5. Biological Factors
The Brain-Body Connection
Biological factors, including neurochemistry and genetics, contribute significantly to mental health. The intricate interplay between neurotransmitters, hormones, and genetic predispositions shapes an individual’s susceptibility to mental health conditions and their response to interventions.
6. Environmental Influences
Contextual Impact
The environment in which an individual lives, works, and grows plays a crucial role in mental health. Factors such as socioeconomic status, access to resources, cultural norms, and exposure to trauma can profoundly influence mental well-being.
7. Spiritual Well-Being
Connecting Beyond the Physical
Spiritual well-being involves finding meaning, purpose, and connection beyond the material aspects of life. For many individuals, spirituality provides a source of solace, guidance, and a framework for understanding the broader context of their existence.
8. Balancing Work and Leisure
The Importance of Work-Life Harmony
The delicate balance between work and leisure contributes to mental health. High levels of stress due to work-related pressures or the absence of fulfilling leisure activities can impact mental well-being. Striking a harmonious balance is essential for sustained mental health.
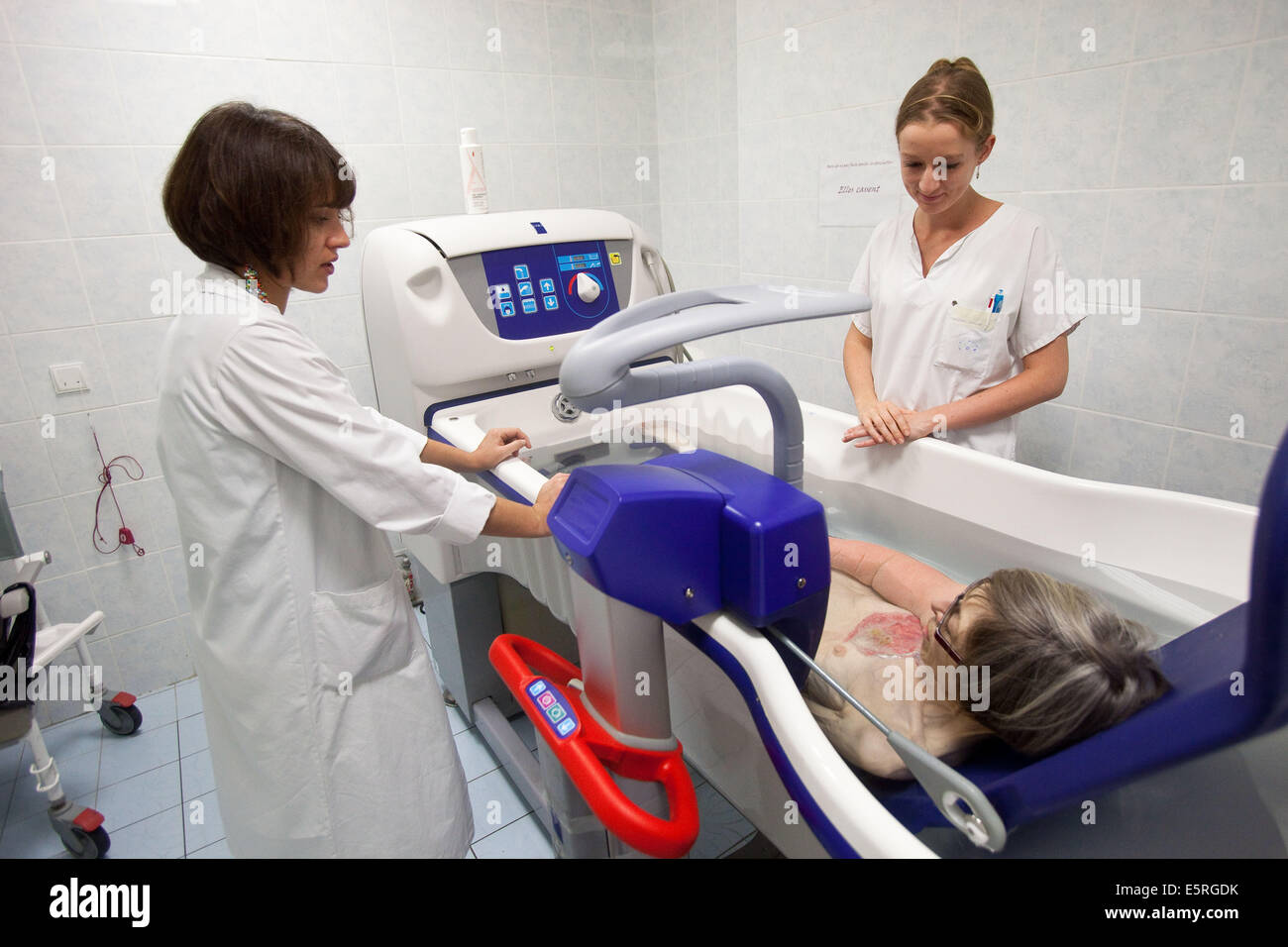
9. Access to Mental Health Care
Breaking Barriers to Support
Access to mental health care is a critical aspect of mental well-being. Removing barriers to seeking professional help, promoting mental health awareness, and ensuring the availability of mental health services contribute to a supportive and inclusive mental health landscape.
In Conclusion
Mental health is a multifaceted construct influenced by various interconnected aspects of life. Recognizing and addressing these dimensions collectively contribute to fostering a society that values and prioritizes the mental well-being of its individuals.
FAQs
- How can I improve my emotional well-being?
- Improving emotional well-being involves self-awareness, practicing mindfulness, seeking support from loved ones, and considering professional assistance if needed.
- What factors contribute to psychological resilience?
- Factors contributing to psychological resilience include positive social connections, effective coping strategies, a growth mindset, and a sense of purpose.
- Can biological factors be modified for better mental health?
- While genetic predispositions are inherent, lifestyle choices, including exercise, nutrition, and stress management, can positively influence biological factors for better mental health.
- How does spirituality impact mental well-being?
- Spirituality provides a framework for finding meaning and connection, offering individuals a source of comfort, purpose, and a broader perspective on life’s challenges.
- Why is work-life balance crucial for mental health?
- Striking a balance between work and leisure prevents burnout, reduces stress, and ensures individuals have time for activities that bring joy and fulfillment, contributing to overall mental well-being.