Cholelithiasis, commonly known as gallstones, refers to the formation of solid particles, or stones, in the gallbladder or bile ducts. These stones may vary in size and composition and can cause a range of symptoms and complications. Cholelithiasis can be asymptomatic or lead to acute or chronic conditions such as cholecystitis (inflammation of the gallbladder), biliary colic (episodic pain in the upper abdomen), or choledocholithiasis (stones in the common bile duct).
Factors contributing to the development of gallstones include obesity, rapid weight loss, a high-fat diet, certain medications, and genetic predisposition. Treatment options for cholelithiasis may include dietary modifications, medications to dissolve stones, or surgical removal of the gallbladder (cholecystectomy), depending on the severity of symptoms and associated complications. Early diagnosis and appropriate management are essential to prevent complications and improve patient outcomes.
Table of Contents
ToggleFormation of Gallstones
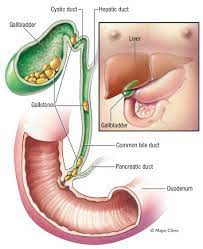
Gallstones are solid formations resembling pebbles that develop within the gallbladder. They can vary in size, ranging from as small as a grain of sand to as large as a golf ball. Gallstones form when bile, a digestive fluid stored in the gallbladder, undergoes a process of hardening into stone-like material.
Bile comprises water, cholesterol, fats, bile salts, proteins, and bilirubin, a waste product. When the composition of bile becomes imbalanced, with elevated levels of cholesterol or bilirubin or decreased bile salts, it becomes prone to solidification and gallstone formation.
The precise reasons for these imbalances are not fully understood. However, factors such as diet, obesity, genetics, and certain medical conditions may contribute to the development of gallstones. Understanding the mechanisms underlying gallstone formation is crucial for prevention and management strategies aimed at reducing the risk of complications associated with this condition.
There are two primary types of gallstones:
- Cholesterol Stones: These gallstones are composed of hardened cholesterol and represent the most prevalent type. Typically yellow-green in color, cholesterol stones form when there is an excess of cholesterol in the bile.
- Pigment Stones: These stones develop from an accumulation of bilirubin in the bile. Pigment stones are generally small and dark in color. Excessive bilirubin levels can lead to the formation of these stones.
The incidence of cholelithiasis and choledocholithiasis impacts individuals of all genders and can occur at any age. However, there is a higher prevalence among females compared to males. Additionally, the likelihood of developing these conditions tends to increase with age, particularly beyond the age of 40. Factors such as hormonal fluctuations, pregnancy, obesity, and certain medical conditions may contribute to the higher incidence observed in females.
While cholelithiasis and choledocholithiasis can affect individuals across the lifespan, older age groups are more commonly affected due to factors such as changes in metabolism, decreased gallbladder function, and a higher likelihood of comorbidities associated with gallstone formation. Understanding the demographics and risk factors associated with cholelithiasis and choledocholithiasis is essential for early detection, prevention, and effective management of these conditions.
Cause
The exact cause of gallstones is not completely understood. However, they often develop in individuals with certain underlying conditions, such as liver cirrhosis, infections of the biliary tract, or hereditary blood disorders like sickle cell anemia. In cases of liver cirrhosis, there may be an imbalance in bile composition, leading to the formation of gallstones. Similarly, biliary tract infections can disrupt the normal function of the gallbladder and bile ducts, increasing the risk of stone formation.
Additionally, hereditary blood disorders like sickle cell anemia can cause the liver to produce excessive bilirubin, which contributes to the development of gallstones. While these factors are known to increase the likelihood of gallstone formation, the precise mechanisms underlying their association require further research for a complete understanding.
Risk Factors for Gallstone Formation
Several factors increase the risk of developing gallstones, including:
- Sex: Women are twice as likely as men to develop gallstones, partly due to hormonal influences. Excessive estrogen levels from factors like pregnancy, hormone replacement therapy, and contraceptive pills can raise cholesterol levels in bile and decrease gallbladder movement, predisposing to gallstone formation.
- Family History: Gallstones often have a familial tendency, with a family history of the condition increasing the risk.
- Obesity: Being overweight, especially moderately, raises the risk of gallstones. This may be because excess weight reduces the amount of bile salts in bile, leading to higher cholesterol levels and decreased gallbladder emptying.
- Diet: Diets high in fat and cholesterol and low in fiber contribute to gallstone formation by increasing cholesterol levels in bile and impairing gallbladder function.
- Rapid Weight Loss: Prolonged fasting or rapid weight loss can lead to gallstone formation as the liver secretes extra cholesterol into bile during fat metabolism, and the gallbladder may not empty properly.
- Age: Individuals over 60 years old are more susceptible to gallstones, as aging is associated with increased cholesterol secretion into bile.
- Ethnicity: Certain ethnicities, such as American Indians, have a genetic predisposition to secrete high levels of cholesterol in bile, increasing the risk of gallstones.
- Cholesterol-Lowering Drugs: Medications that lower blood cholesterol levels can raise the amount of cholesterol secreted into bile, thereby increasing the risk of gallstones.
- Diabetes: People with diabetes often have elevated levels of fatty acids called triglycerides, which can increase the risk of gallstone formation.
- Signs and Symptoms of Gallstones
As gallstones obstruct the bile ducts, pressure builds up in the gallbladder, leading to various symptoms. These signs and symptoms may manifest suddenly, often following fatty meals and sometimes occurring at night. Common indications of gallstone-related issues include:
- Pain in the Right Upper or Middle Upper Abdomen:
- The pain may be intermittent, coming and going, and can vary in intensity from sharp, cramping sensations to dull aches.
- It may radiate to the back or below the right shoulder blade.
- Onset of pain typically occurs within minutes of consuming a meal, particularly one high in fat.
- Fever and chills:
- Gallstone-related blockages can lead to inflammation and infection, resulting in fever, even if it’s low-grade, and chills.
- Yellowish Discoloration of the Skin and Sclera (Jaundice):
- Obstruction of the bile ducts by gallstones can cause bile to accumulate in the bloodstream, leading to jaundice, characterized by yellowing of the skin and the whites of the eyes.
- Abdominal Fullness:
- Patients may experience a sensation of abdominal fullness or discomfort, often accompanied by bloating.
- Clay-Colored Stools:
- Blockage of the bile ducts can affect the normal coloration of stools, resulting in pale or clay-colored feces.
- Nausea and vomiting:
- Nausea and vomiting may occur as a result of gallstone-related symptoms, often in response to pain or digestive disturbances.
- Fat Intolerance:
- Gallstone-related issues can lead to fat intolerance, causing symptoms such as indigestion, abdominal pain, bloating, and excessive belching after consuming fatty foods.
Medical Management
Medical History
- Inquire about the patient’s medical history, including any previous episodes of abdominal pain, jaundice, or digestive issues.
- Ask about risk factors such as obesity, family history of gallstones, and recent changes in diet or weight.
- Obtain information about past medical conditions, surgeries, and medications, especially those known to affect the gallbladder or bile ducts.
Symptom Assessment
- Assess the nature, location, severity, and duration of abdominal pain, especially if it occurs after meals or at night.
- Inquire about associated symptoms such as fever, nausea, vomiting, bloating, and changes in bowel habits, including stool color.
- Determine if the patient has experienced jaundice or other signs of liver dysfunction, such as dark urine or itching.
Dietary History
- Ask about the patient’s dietary habits, particularly their intake of fatty foods and how meals affect their symptoms.
- Inquire about any recent rapid weight loss or dietary changes that may have triggered symptoms.
Physical Examination
- Perform a thorough abdominal examination to assess for tenderness, guarding, or rebound tenderness, especially in the right upper quadrant.
- Palpate the abdomen to check for masses, distension, or enlarged organs such as the liver or spleen.
- Look for signs of jaundice, such as yellowing of the skin or sclera, and examine the eyes for scleral icterus.
- Assess vital signs, including temperature, pulse rate, blood pressure, and respiratory rate, noting any abnormalities suggestive of infection or systemic illness.
- Evaluate for Murphy’s sign, where deep inspiration causes abrupt cessation of inspiration due to pain upon palpation of the gallbladder during inspiration.
- Perform a thorough physical examination to rule out other possible causes of abdominal pain and jaundice, such as liver disease, pancreatitis, or gastrointestinal disorders.
Diagnostic Investigations for Gallstones
- Abdominal Ultrasound:
- Abdominal ultrasound is the preferred initial imaging modality for detecting gallstones. It provides detailed visualization of the gallbladder and biliary tract, allowing for the identification of gallstones based on their location, size, and number. This test is highly sensitive and specific for diagnosing gallstones.
- Computerized Tomography (CT) Scan:
- A CT scan is a non-invasive imaging technique that generates cross-sectional images of the body. It may be used to identify gallstones and assess for complications such as infection, inflammation, or rupture of the gallbladder or bile ducts.
- Cholecystography:
- Cholecystography involves injecting a small amount of non-harmful radioactive material into the patient, which is absorbed by the gallbladder. X-rays are then taken to visualize the gallbladder and detect gallstones, which appear as dark spots against the opaque background of the gallbladder.
- Endoscopic Retrograde Cholangiopancreatography (ERCP):
- ERCP is a procedure used to locate and remove stones in the bile ducts. It involves inserting an endoscope through the mouth, esophagus, stomach, and into the small intestine. A special dye is injected to visualize the bile ducts and gallstones on a monitor. Stones can then be captured and removed using specialized tools attached to the endoscope.
- Blood Tests:
- Various blood tests may be performed to assess for signs of gallstone-related complications, such as infection, obstruction, pancreatitis, or jaundice. These tests may include measurement of bilirubin levels, liver function tests (e.g., ALT, AST, ALP), and pancreatic enzymes (e.g., amylase, lipase).
Treatment
- Oral Dissolution Therapy:
- Chenodeoxycholic Acid (CDCA, Chenodiol): Used for the dissolution of cholesterol stones, typically those smaller than 20mm in diameter. The initial dosage is 250mg orally twice daily for the first 2 weeks, with weekly increases of 250 mg/day, up to 13 to 16 mg/kg/day for up to 24 months.
- Ursodeoxycholic Acid (UDCA, Ursodiol, Actigall): Also used for dissolving cholesterol gallstones less than 20mm in diameter, particularly when surgery is not feasible. The typical dosage is 8 to 10 mg/kg orally daily, divided into two or three doses, for 12 to 24 months.
- Contact Dissolution Therapy:
- Methyl tert-butyl ether: Still under experimental use, this drug is injected directly into the gallbladder to dissolve cholesterol stones. Research is ongoing to evaluate its efficacy and safety.
- Symptomatic Management:
- Analgesics: Opioid analgesics are administered to alleviate pain associated with gallstone attacks.
- Antispasmodics or anticholinergics: These medications help decrease secretions and counteract smooth muscle spasms, thereby relieving symptoms such as abdominal pain. Dicyclomine is an example of such a medication.
- Antiemetics: Used to control nausea and vomiting, which may occur during gallstone attacks.
- Antibiotics: prescribed to eliminate infection if present, particularly in cases of acute cholecystitis or cholangitis.
- Surgical Intervention:
- If conservative treatments fail or if there are complications, surgical intervention may be necessary. Surgical options include:
- Cholecystectomy: Surgical removal of the gallbladder is the standard treatment for symptomatic gallstones.
- Cholecystostomy: In emergency situations, an incision may be made into the gallbladder to remove stones, particularly if the patient is not stable enough for elective surgery.
- If conservative treatments fail or if there are complications, surgical intervention may be necessary. Surgical options include:
Nursing Management
Objectives of Management:
Pain Management: The primary aim is to effectively control the pain associated with gallstone attacks using analgesic medications to improve patient comfort and quality of life.
Infection Control: The administration of antibiotics is essential to treat and prevent infection, particularly in cases of acute cholecystitis or cholangitis, thereby reducing the risk of complications and promoting recovery.
Fluid and Electrolyte Balance Maintenance: Maintaining optimal fluid and electrolyte balance is crucial for overall patient well-being. Adequate hydration and monitoring of electrolyte levels help prevent dehydration and ensure proper physiological functioning.
Environment
- Interventions:
- Maintain a safe and comfortable environment conducive to patient recovery and well-being.
- Ensure adequate ventilation and temperature control to promote comfort and prevent overheating or chilling.
- Minimize noise and disruptions to facilitate rest and sleep for the patient.
- Regularly assess the cleanliness and organization of the patient’s room and equipment, addressing any issues promptly.
Observation
- Interventions:
- Conduct regular assessments of the patient’s vital signs, including temperature, pulse, respiratory rate, and blood pressure.
- Monitor for signs of complications, such as fever, jaundice, abdominal distention, or changes in mental status.
- Document observations accurately and promptly report any concerning findings to the healthcare team.
- Educate the patient and family on self-monitoring techniques and when to seek medical attention for worsening symptoms.
Psychological Care
- Interventions:
- Provide emotional support and reassurance to the patient and family members, acknowledging their concerns and addressing any fears or anxieties.
- Encourage open communication and active listening, allowing the patient to express their feelings and concerns.
- Offer information and resources on coping strategies, relaxation techniques, and support groups for patients dealing with chronic illness.
- Collaborate with mental health professionals as needed for additional support and counseling.
Hygiene
- Interventions:
- Assist the patient with personal hygiene activities, such as bathing, grooming, and oral care, as needed.
- Ensure the availability of clean linens, towels, and toiletries to maintain cleanliness and comfort.
- Educate the patient on proper handwashing techniques and hygiene practices to prevent the spread of infection.
- Monitor skin integrity and provide interventions to prevent pressure ulcers and skin breakdown.
Exercises
- Interventions:
- Collaborate with physical therapists to develop an individualized exercise program tailored to the patient’s abilities and limitations.
- Encourage regular physical activity, such as walking or range of motion exercises, to promote circulation, strength, and mobility.
- Provide education on safe and appropriate exercise techniques, emphasizing the importance of gradual progression and avoiding overexertion.
- Monitor the patient’s response to exercise and adjust the program as needed based on their tolerance and goals.
Nutrition
- Interventions:
- Assess the patient’s nutritional status and dietary preferences to develop a customized meal plan that meets their needs and restrictions.
- Offer regular, small meals and snacks to maintain energy levels and prevent nutritional deficiencies.
- Provide education on healthy eating habits, portion control, and the importance of a balanced diet rich in fruits, vegetables, lean proteins, and whole grains.
- Collaborate with dietitians or nutritionists to address specific dietary concerns, such as food intolerances, allergies, or malnutrition.
Elimination
- Interventions:
- Monitor bowel and bladder function regularly, assessing for any changes or abnormalities in frequency, consistency, or volume.
- Encourage adequate fluid intake to support hydration and promote regular bowel movements.
- Provide assistance with toileting and personal hygiene as needed, ensuring privacy and dignity for the patient.
- Implement strategies to prevent constipation or urinary retention, such as dietary modifications, fiber supplementation, and regular toileting schedules.
Medication
- Interventions:
- Administer prescribed medications accurately and on schedule, adhering to proper dosage and administration routes.
- Monitor for adverse reactions or side effects of medications, such as allergies, gastrointestinal upset.
Complications of Cholelithiasis
- Gallbladder Infection:
- The presence of gallstones in the gallbladder can increase the risk of bacterial infection, leading to acute cholecystitis. Infection may occur if the bile flow is obstructed by gallstones, allowing bacteria to multiply within the gallbladder.
- Gallbladder Rupture:
- Severe inflammation or pressure from gallstones can cause the gallbladder to rupture, resulting in a medical emergency. Gallbladder rupture can lead to peritonitis, a life-threatening condition characterized by inflammation of the abdominal cavity.
- Acute Cholecystitis:
- Gallstones that become lodged in the neck of the gallbladder can cause inflammation and swelling, resulting in acute cholecystitis. This condition is marked by severe abdominal pain, fever, and tenderness in the upper right abdomen.
- Gallbladder Cancer:
- Prolonged irritation and inflammation of the gallbladder wall caused by gallstones may increase the risk of developing gallbladder cancer, although this complication is relatively rare.
- Pancreatitis:
- Gallstones can block the pancreatic duct, leading to inflammation of the pancreas known as pancreatitis. Pancreatitis is a serious condition characterized by severe abdominal pain, nausea, vomiting, and elevated pancreatic enzymes in the blood.
- Small Bowel Obstruction:
- Large gallstones may migrate from the gallbladder and become lodged in the small intestine, leading to obstruction. Small bowel obstruction can cause symptoms such as abdominal pain, bloating, vomiting, and constipation.
- Obstructive Jaundice:
- Gallstones that obstruct the bile ducts can impair the flow of bile from the liver to the intestine, resulting in obstructive jaundice. This condition is characterized by yellowing of the skin and eyes, dark urine, and pale stools due to the accumulation of bilirubin in the bloodstream.
Read more: Medical-Surgical Nursing
Read more: Liver cirrhosis | Causes | Pathophysiology | Signs and symptoms | Treatment | Nursing Management








[…] Read more: Cholelithiasis | Cause | Signs and Symptoms | Treatment | Nursing Management […]