A newborn involves marveling at intricate, involuntary responses wired into the infant nervous system. These automatic movements, newborn reflexes, also known as primitive reflexes, support feeding, protection, and early motor patterns while cortical networks mature. For nurses and perinatal teams, skilled evaluation of reflexes provides crucial information about brain and spinal cord function, helps distinguish normal variation from pathology, and guides parent education with clarity and confidence.
This in-depth, nurse-led guide explains what each reflex indicates, how to elicit it safely, when it should appear and integrate, and which findings warrant further evaluation. The goal: translate neurodevelopment into practical bedside care.
Newborn Reflexes: Moro, Rooting, Sucking, Grasp & More | Assessment, Timeline, and Nursing Care
Newborn Reflexes at a Glance
Primitive reflexes are brainstem- and spinal cord–mediated movements present at birth or shortly thereafter. Many integrate within the first months as voluntary control increases, while protective extensions emerge later and persist.
Key points:
- Reflexes are adaptive in early life (feeding, protection, alignment).
- Integration timelines vary with gestational age and health status.
- Asymmetry, absence, or persistence beyond expected ages may signal neurologic or musculoskeletal concerns and requires appropriate follow-up.
Why Newborn Reflexes Matter in Nursing Practice
- Neurologic screening: Reflex quality (present, symmetric, brisk, fatigable) offers insight into central and peripheral nervous system integrity.
- Developmental trajectory: Expected integration aligns with rising cortical control; delayed integration can interfere with posture, feeding, and motor milestones.
- Early detection: Abnormal patterns may reflect brachial plexus injury, clavicle fracture, intracranial pathology, hypoxic-ischemic encephalopathy, or metabolic concerns.
- Parent education: Clear, anticipatory guidance reduces anxiety and improves engagement in care plans.
Neurodevelopment Essentials for Context
- Subcortical dominance: In the neonatal period, brainstem circuits drive automatic responses; frontal cortical inhibition strengthens across infancy.
- Myelination and synaptic refinement: Rapid first-year maturation supports reflex integration and purposeful movement.
- Gestational age effect: Preterm infants often display immature, inconsistent reflexes that organize with time; assessment must account for corrected age.
Summary Table—Common Newborn Reflexes, Onset, and Integration
| Reflex | Stimulus | Normal Response | Typical Onset | Integration (Resolution) | Notes |
| Rooting | Stroke corner of mouth/cheek | Head turns toward stimulus; mouth opens | Present at birth (develops by ~32–36 wks GA) | ~3–4 months | Supports latch and feeding |
| Sucking/Swallowing | Nipple/finger to lips or palate | Rhythmic suck, swallow, breathe coordination | Present at birth (matures 34–37 wks GA) | ~3–4 months (becomes voluntary) | Fatigue or discoordination suggests prematurity or illness |
| Moro (Startle) | Sudden head drop or loud noise | Extension-abduction of arms with opening of hands, then flexion/adduction | Present at birth (complete by term) | ~4–6 months | Asymmetry suggests brachial plexus injury or fracture |
| Palmar Grasp | Pressure in palm | Finger flexion; strong grasp | Present at birth | ~4–6 months | Persistence may impede purposeful reach |
| Plantar Grasp | Pressure to ball of foot | Toe flexion | Present at birth | ~9–12 months | Persistence may affect standing balance |
| Babinski (Extensor Plantar) | Stroke lateral sole to toes | Toe fanning; big toe dorsiflexes | Present at birth | ~12 months (may persist up to 24 months) | Normal in infants; abnormal beyond toddler period |
| ATNR (Tonic Neck/Fencer’s) | Turn head to one side | Extension of arm/leg on face side; flexion on skull side | Present at birth | ~4–6 months | Asymmetry may indicate ipsilateral weakness |
| Stepping/Automatic Walking | Upright hold, feet touch surface | Alternating “steps” | Present at birth | ~1–2 months (reappears as voluntary walking later) | Disappears as limb weight increases relative to strength |
| Galant (Trunk Incurvation) | Stroke paraspinal area | Lateral trunk flexion toward stimulus | Present at birth | ~2–4 months | Asymmetry suggests spinal lesion |
| Crawling (Bauer) | Prone position, gentle pressure to soles | Crawling-like movements | Present at birth | ~2 months | Precursor to later volitional prone mobility |
| Landau | Ventral suspension | Head extends, trunk straightens, legs extend | ~3–4 months | ~12–24 months | Emergent postural control |
| Parachute (Protective Extension) | Quick forward descent in sitting | Arms extend forward to protect | ~6–9 months | Persists | Protective, not primitive; absence raises concern after 9 months |
GA = gestational age.
How to Examine Newborn Reflexes Safely and Effectively
Preparation and Setting
- Environment: Warm, quiet, and softly lit room reduces startle and supports accurate observation.
- State: Best during quiet alert or light sleep for some reflexes; avoid deep sleep or active crying when feasible.
- Timing: Perform between feeds to minimize regurgitation and irritability.
- Infection prevention: Hand hygiene and clean equipment are essential.
- Positioning: Provide head and neck support; use a firm, flat surface for supine or prone assessments; ensure safe swaddling as needed.
Documentation Framework
- Presence and symmetry: Present/absent, left vs right, upper vs lower limbs.
- Quality and threshold: Brisk vs depressed; stimulus intensity required; fatigability.
- Timing: Consistency across the exam; response amplitude after repeated stimuli.
- Developmental context: Gestational and corrected age, perinatal history, medications, and feeding status.
Detailed Guide to Major Newborn Reflexes
Rooting Reflex
- Stimulus: Stroke the corner of the mouth or cheek.
- Response: The infant turns the head toward the stimulus and opens the mouth, seeking to latch.
- Onset/Integration: Present at birth; integrates by about 3–4 months as voluntary oromotor control emerges.
- Clinical notes:
- Essential for early feeding; weak rooting may follow sedation, maternal medications, or prematurity.
- Asymmetry can indicate facial nerve involvement or localized trauma.
- Nursing tips: Encourage skin-to-skin contact and early feeding cues; provide lactation support for latch difficulties.
Sucking and Swallowing Reflex
- Stimulus: Nipple or clean finger to lips or palate.
- Response: Rhythmic suck with coordinated swallow-breathe pattern.
- Onset/Integration: Begins ~32–34 weeks GA, matures near term; integrates by ~3–4 months transitioning to voluntary control.
- Clinical notes:
- Discoordination may indicate prematurity, central nervous system depression, or structural anomalies (e.g., cleft palate).
- Pulse oximetry and careful pacing can support safe oral feeds in late preterm infants.
- Nursing tips: Assess suck-swallow-breathe rhythm; teach paced feeding strategies as appropriate.
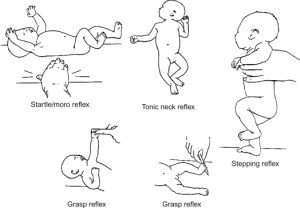
Moro (Startle) Reflex
- Stimulus: Sudden head extension (gentle, controlled) or unexpected loud sound.
- Response: Rapid shoulder abduction and elbow extension with finger splay, followed by flexion and adduction; often accompanied by a brief cry.
- Onset/Integration: Present at birth; integrates by ~4–6 months.
- Clinical notes:
- Asymmetric Moro suggests brachial plexus injury, clavicular fracture, or hemiparesis.
- Exaggerated Moro may occur with hypocalcemia or drug withdrawal.
- Diminished Moro may reflect CNS depression or severe illness.
- Safety: Support the head and neck; avoid undue cervical stress.
Palmar Grasp Reflex
- Stimulus: Pressure on the palmar surface.
- Response: Finger flexion with a strong grasp that may briefly support body weight.
- Onset/Integration: Present at birth; integrates by ~4–6 months.
- Clinical notes:
- Persistence can impede voluntary release and reaching.
- Asymmetry may indicate peripheral nerve involvement.
- Nursing tips: Observe for coordinated transition from reflex grasp to purposeful hand use around 4–6 months.
Plantar Grasp Reflex
- Stimulus: Pressure to the plantar surface at the metatarsal heads.
- Response: Toe flexion.
- Onset/Integration: Present at birth; integrates by ~9–12 months.
- Clinical notes:
- Excess persistence can affect shoe wear and early standing balance.
- Often present longer than palmar grasp; interpret within developmental context.
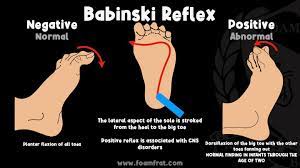
Babinski (Extensor Plantar) Reflex
- Stimulus: Firm stroke along the lateral sole toward the toes.
- Response: Toe fanning with dorsiflexion of the great toe.
- Onset/Integration: Present at birth; integrates by ~12 months, occasionally up to 24 months.
- Clinical notes:
- Normal extensor response in infants; flexor plantar response emerges with corticospinal maturation.
- Extensor response after toddler period warrants evaluation.
Asymmetric Tonic Neck Reflex (ATNR, “Fencer”)
- Stimulus: Turn the head to one side while supine.
- Response: Arm and leg on face side extend; opposite limbs flex.
- Onset/Integration: Present at birth; integrates by ~4–6 months.
- Clinical notes:
- Facilitates hand-eye regard and early visual exploration.
- Persistence may interfere with rolling and midline control.
- Marked asymmetry suggests motor weakness or hemiplegia.
Stepping (Automatic Walking) Reflex
- Stimulus: Hold the infant upright, allowing feet to touch a firm surface.
- Response: Alternating “stepping” movements.
- Onset/Integration: Present at birth; integrates by ~1–2 months as limb weight increases relative to strength.
- Clinical notes:
- Reappears later as voluntary stepping near independent walking onset.
- Useful for observing lower limb symmetry and tone.
Galant (Trunk Incurvation) Reflex
- Stimulus: Stroke paraspinal area from shoulder to hip while in ventral suspension or prone.
- Response: Lateral trunk flexion toward the side of stimulation.
- Onset/Integration: Present at birth; integrates by ~2–4 months.
- Clinical notes:
- Asymmetry can reflect spinal or peripheral nerve involvement.
- Useful during assessments for spinal dysraphism signs.
Crawling (Bauer) Reflex
- Stimulus: Place in prone; apply gentle pressure to soles.
- Response: Alternating limb movements resembling crawling.
- Onset/Integration: Present at birth; integrates by ~2 months.
- Clinical notes:
- Precursor to voluntary prone mobility; absence alone is not diagnostic.
- Observe in a warm, calm environment to avoid suppression by distress.
Landau Reaction
- Stimulus: Horizontal ventral suspension.
- Response: Head extends, back straightens, hips extend.
- Onset/Integration: Emerges ~3–4 months; integrates by ~12–24 months.
- Clinical notes:
- Absence may signal hypotonia; exaggerated response may appear with hypertonia.
Parachute (Protective Extension) Reflex
- Stimulus: Quick forward displacement while sitting or ventral suspension.
- Response: Arms extend forward with hand opening to protect.
- Onset/Integration: Appears ~6–9 months; persists through life as a protective response.
- Clinical notes:
- Absence after 9 months raises concern for motor delay or neuromuscular disorders.
Blink and Gag Reflexes (Protective, Persistent)
- Stimulus: Sudden bright light or corneal touch (blink); posterior oral stimulation (gag).
- Response: Eye closure; pharyngeal contraction.
- Onset/Integration: Present at birth; persist for life.
- Clinical notes:
- Essential airway and ocular protection; diminished response warrants careful evaluation.
Extrusion (Tongue Thrust) Reflex
- Stimulus: Object or spoon touches anterior tongue.
- Response: Tongue pushes outward.
- Onset/Integration: Present at birth; integrates by ~4–6 months with readiness for solids.
- Clinical notes:
- Persistence may contribute to feeding challenges and delayed acceptance of textures.
Special Considerations in Preterm and Medically Complex Infants
- Corrected age: Interpret reflex maturity using corrected age for preterm infants.
- Respiratory status: Hypoxia, acidosis, and fatigue depress responses; schedule when stable.
- Medication effects: Magnesium sulfate, opioids, and sedatives can dampen reflexes; document context.
- Neuromuscular tone: Hypotonia blunts multiple reflexes; hypertonia may exaggerate them.
- NICU environment: Minimize noxious stimuli; support thermoregulation and pain control during assessments.
Interpreting Abnormal Reflex Findings
Red Flags Requiring Prompt Evaluation
- Absence of multiple primitive reflexes at term-equivalent age.
- Pronounced asymmetry of Moro, palmar grasp, or Galant.
- Persistence of strong primitive reflexes well beyond expected integration (e.g., ATNR after 6 months, Moro after 6 months).
- Extensor plantar (Babinski) beyond toddler period with other upper motor neuron signs.
- Weak or absent suck-swallow with poor coordination at term.
- Ocular signs (sunsetting eyes), seizures, or altered consciousness with abnormal reflex profile.
Differential Diagnosis Clues from Reflex Patterns
- Asymmetric Moro with intact palmar grasp: Consider brachial plexus injury or clavicle fracture.
- Global depression of reflexes: Consider CNS depression, sepsis, metabolic derangements, or medication effects.
- Persistent primitive reflexes with hypertonia: Consider cerebral palsy or other upper motor neuron conditions.
- Absent Galant with midline cutaneous stigmata: Consider spinal dysraphism.
- Weak rooting/suck with micrognathia or cleft: Consider structural causes requiring multidisciplinary care.
Stepwise Nursing Assessment Algorithm
- Prepare: Warm environment, hand hygiene, safe positioning, gather supplies.
- Observe baseline: Tone, posture, spontaneous movement, respiratory pattern, alertness.
- Elicit reflexes methodically:
- Cranial-nerve related (rooting, suck-swallow, blink)
- Brainstem/postural (Moro, ATNR, Galant)
- Spinal/appendicular (palmar/plantar grasp, stepping)
- Document findings: Presence, symmetry, quality, fatigue, and any associated signs.
- Synthesize: Compare with gestational/corrected age and perinatal history.
- Communicate: Share concerns promptly; arrange further evaluation as indicated.
- Educate caregivers: Explain normal ranges and timelines in clear, support-focused language.
Parent Education Points for Care Teams
- Primitive reflexes are normal and expected early in life; most fade as voluntary control develops.
- Startle responses can be strong; secure swaddling (following safe sleep guidance) and quiet environments can reduce overstimulation.
- Feeding reflexes mature across late gestation; lactation support and paced feeding techniques improve coordination.
- Callouts about safety (e.g., head support during handling) help prevent injury during strong Moro responses.
- Encourage routine well-child visits where reflexes and development are monitored.
Note: Provide education using inclusive, nonjudgmental language and culturally responsive approaches.
Interprofessional Collaboration and Referral
- Pediatrics/Neonatology: Persistent or absent reflexes, hypotonia/hypertonia, or seizure concerns.
- Physical/Occupational Therapy: Motor patterning, positioning, and early intervention services.
- Speech-Language Pathology: Feeding and swallow assessment when suck-swallow-breathe coordination is suboptimal.
- Neurology: Refractory abnormalities, suspected seizure activity, or regression.
- Orthopedics/Physiatry: Brachial plexus injury, fractures, or musculoskeletal asymmetries.
- Lactation Consultants: Latch, milk transfer, and feeding endurance issues.
Practical Tips to Improve Accuracy and Comfort
- Warm hands and gentle touch prevent withdrawal from cold stimuli.
- Use consistent stimulus intensity; avoid repeated strong stimuli that provoke fatigue.
- Support the head during Moro testing; use a controlled, minimal head-drop motion.
- During suck evaluation, monitor for color change, nasal flaring, or desaturation; pause as needed.
- Integrate reflex testing into routine care to minimize handling bursts.
Quality, Safety, and Equity Considerations
- Trauma-informed care: Announce actions, proceed at an unhurried pace, and allow pauses.
- Equity: Provide language-concordant education, use interpreters, and respect cultural newborn care practices while maintaining safety.
- Documentation: Time-stamped entries with context (e.g., immediately post-feed, on magnesium sulfate) support clinical reasoning and handoffs.
- Safe sleep: Reinforce supine sleep and crib safety while teaching calming strategies for strong startle responses.
Case Snapshots for Clinical Context
- Case 1: Term infant with exaggerated, symmetric Moro and mild tremulousness after a prolonged labor. Electrolytes show low calcium; treatment normalizes reflex intensity within 24 hours.
- Case 2: Newborn with absent Moro on the right, intact palmar grasp bilaterally, and tenderness over the clavicle. Imaging confirms clavicle fracture; conservative management with positioning leads to resolution as healing progresses.
- Case 3: Late preterm infant with weak suck and poor feeding endurance. Coordinated plan with lactation and speech-language pathology introduces paced feeding and side-lying positioning; weight gain stabilizes and suck strength improves by due date.
Evidence and Guidelines Snapshot
- Pediatric neurologic examination standards emphasize symmetry, graded responses, and developmental context.
- AAP and neonatology texts outline expected timelines and when to escalate evaluation.
- WHO and neonatal care manuals provide guidance on preterm adaptations and feeding reflex maturity.
Citations in a clinical policy or local guideline document can expand on these foundations, ensuring alignment with regional practice.
Frequently Asked Questions (FAQ)
What are the most important newborn reflexes checked after birth?
Commonly assessed reflexes include Moro (startle), rooting, sucking/swallowing, palmar and plantar grasp, Babinski (extensor plantar), ATNR (tonic neck), stepping, and Galant. Protective reactions like blink and gag are also observed.
When do newborn reflexes typically disappear?
Many integrate within months: rooting and sucking by ~3–4 months; Moro and ATNR by ~4–6 months; plantar grasp by ~9–12 months; Babinski by ~12 months (sometimes up to 24 months). Parachute reactions appear around 6–9 months and persist.
What does asymmetric reflex activity indicate?
Marked asymmetry, especially in Moro, grasp, or Galant, can indicate peripheral nerve injury, clavicle fracture, hemiparesis, or localized musculoskeletal issues. Symmetry across limbs is a key marker of neurologic health.
Do premature infants have different reflex timelines?
Yes. Reflexes may be less consistent in preterm infants and often organize with corrected age. Feeding reflexes, in particular, mature across late gestation; assessment should consider respiratory stability and fatigue.
How are newborn reflexes tested safely?
Testing occurs in a warm, calm setting with head and neck support. Stimuli are delivered gently and consistently, with careful observation for color changes, breathing effort, and fatigue. Documentation includes presence, symmetry, and quality.
Conclusion
Newborn Reflexes provide a window into early neural circuitry, offering a fast, reliable snapshot of brainstem and spinal function while higher cortical systems mature. Thorough, consistent assessment paired with clear documentation and timely referral when findings deviate from expected patterns elevates safety and supports optimal development. Nursing teams translate complex neurobiology into practical bedside care, strengthen family understanding through precise education, and coordinate interdisciplinary support that turns early observations into long-term gains for infant health.
Educational Note: Content is designed for professional education and does not replace individualized clinical assessment or local protocols.