What is bronchiectasis?
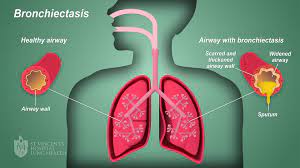
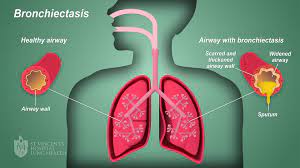
Bronchiectasis is a respiratory condition characterized by the abnormal widening and thickening of the bronchial tubes, resulting in their permanent dilation.
This disorder affects the respiratory system and can arise from various causes, including recurrent respiratory infections, cystic fibrosis, immunodeficiency disorders, and airway obstruction.
Two prominent features of bronchiectasis are chronic coughing, often accompanied by the production of excessive sputum, and recurrent respiratory infections due to the impaired clearance of mucus from the dilated bronchial tubes.
These characteristics significantly impact the quality of life of individuals with bronchiectasis and necessitate ongoing management and treatment to alleviate symptoms and prevent complications.
Causes of Bronchiectasis
- Microorganisms: Viruses and Bacteria Bronchiectasis often arises from the repeated onslaught of respiratory infections caused by various microorganisms, such as viruses and bacteria. These pathogens invade the respiratory tract, leading to chronic inflammation and structural damage to the bronchial tubes over time.
- Cystic Fibrosis A prevalent underlying cause of bronchiectasis is cystic fibrosis, a genetic disorder characterized by the production of thick, sticky mucus in the airways. This abnormal mucus obstructs the bronchial passages, fostering bacterial growth and chronic infection, ultimately contributing to the development of bronchiectasis.
- Obstruction: Foreign Bodies and Tumors Obstruction of the airways, whether by foreign bodies or tumors, can significantly predispose individuals to bronchiectasis. Foreign bodies lodged in the bronchi disrupt airflow and cause localized damage, while tumors may physically block the passage of air, both impairing the normal function of the respiratory system and leading to bronchial dilation.
- Inhalation of Corrosive Gases The inhalation of corrosive gases represents another potential cause of bronchiectasis. Exposure to such agents directly injures the delicate lining of the airways, triggering inflammation and structural changes that contribute to the development of bronchial dilation and subsequent bronchiectasis.
Predisposing factors
- Measles Measles, a highly contagious viral infection, can serve as a predisposing factor for bronchiectasis. The severe respiratory symptoms associated with measles, including coughing and difficulty breathing, can lead to prolonged inflammation and damage to the bronchial tubes, setting the stage for the development of bronchiectasis in susceptible individuals.
- Broncho-pneumonia Bronchopneumonia, a type of bacterial pneumonia that affects the bronchi and surrounding lung tissue, can predispose individuals to bronchiectasis. The inflammatory response triggered by bronchopneumonia can cause scarring and structural changes in the airways, increasing the likelihood of bronchial dilation and subsequent bronchiectasis.
- Chronic Bronchitis Chronic bronchitis, characterized by persistent inflammation of the bronchial tubes and excessive mucus production, is a common predisposing condition for bronchiectasis. The chronic irritation and damage to the airways associated with chronic bronchitis can weaken the bronchial walls, making them more susceptible to dilation and structural changes over time.
- Tuberculosis Tuberculosis (TB), a bacterial infection primarily affecting the lungs, can predispose individuals to bronchiectasis. The destructive nature of TB on lung tissue can result in extensive scarring and fibrosis, leading to narrowing and obstruction of the bronchial passages. These structural changes increase the risk of bronchial dilation and the subsequent development of bronchiectasis in individuals with a history of TB.
Pathophysiology
Bronchiectasis involves a complex interplay of inflammatory processes, structural changes, and impaired mucociliary clearance within the respiratory system.
The condition typically begins with an initial insult, such as recurrent respiratory infections, cystic fibrosis, or airway obstruction, which triggers inflammation in the bronchial tubes.
Chronic inflammation leads to damage of the bronchial walls and surrounding tissues, resulting in the weakening and dilation of the airways.
This bronchial dilation is accompanied by the accumulation of thickened mucus, which further obstructs airflow and creates an environment conducive to bacterial colonization and recurrent infections.
Over time, the persistent cycle of inflammation, infection, and mucus production contributes to the progressive destruction of the bronchial architecture, leading to irreversible bronchiectasis.
The dilated and distorted bronchial tubes lose their ability to effectively clear mucus and pathogens, perpetuating the cycle of inflammation and infection.
Additionally, the presence of bronchiectasis can exacerbate respiratory symptoms and impair lung function, leading to chronic cough, excessive sputum production, and recurrent respiratory infections.
Complications such as respiratory failure, pneumonia, and lung abscesses may arise in severe cases.
Signs and Symptoms
Bronchiectasis manifests with a variety of signs and symptoms, reflecting the underlying pathophysiological changes within the respiratory system.
- Chronic Cough with Large Amounts of Purulent Sputum: One of the hallmark symptoms of bronchiectasis is a persistent cough, often accompanied by the production of copious amounts of thick, purulent sputum. This occurs due to the impaired clearance of mucus from the dilated bronchial tubes, leading to its accumulation and subsequent coughing as the body attempts to expel the excess secretion.
- Haemoptysis: Bronchiectasis can cause episodes of haemoptysis, or coughing up blood, due to the inflammation and damage to the bronchial walls. The dilation of the bronchi increases the likelihood of blood vessels rupturing, resulting in the presence of blood in the sputum.
- Clubbing of the Fingers: Clubbing of the fingers, characterized by the enlargement and rounding of the fingertips, is a physical manifestation commonly associated with chronic respiratory conditions, including bronchiectasis. It occurs due to chronic hypoxia and tissue inflammation, leading to changes in the structure of the nail beds and fingertips.
- Loss of Energy, Appetite, and Weight: Bronchiectasis can lead to systemic symptoms such as fatigue, decreased appetite, and unintentional weight loss. These symptoms may result from the body’s increased metabolic demands due to chronic inflammation, as well as the energy expenditure associated with coughing and respiratory efforts.
- Fever and Sweating at Times: Episodes of fever and sweating may occur in individuals with bronchiectasis, particularly during periods of acute exacerbation or respiratory infection. These symptoms are indicative of the body’s immune response to infection and inflammation within the respiratory tract.
- Shortness of Breath: Patients with bronchiectasis often experience shortness of breath, especially during physical exertion or exacerbations of their condition. This symptom occurs due to the narrowing and obstruction of the airways, which impairs the normal flow of air in and out of the lungs.
- Chest Pain: Chest pain may occur in some patients with bronchiectasis, particularly during acute exacerbations or due to underlying respiratory infections. The inflammation and irritation of the bronchial tubes can lead to discomfort or aching sensations in the chest area.
- Wheezing: Wheezing, characterized by high-pitched whistling sounds during breathing, can occur in individuals with bronchiectasis. This symptom results from turbulent airflow through narrowed or obstructed bronchial passages.
- Fatigue and Weakness: Chronic fatigue and weakness are common symptoms of bronchiectasis, often attributed to the body’s response to chronic inflammation, frequent coughing episodes, and respiratory infections. These symptoms can significantly impact daily activities and the overall quality of life.
- Recurrent Respiratory Infections: Bronchiectasis predisposes patients to recurrent respiratory infections, such as bronchitis, pneumonia, and sinusitis. Frequent episodes of infection contribute to worsening symptoms and exacerbations of the underlying condition.
- Breathlessness While Lying Flat (Orthopnea): Patients with bronchiectasis may experience difficulty breathing when lying flat, a condition known as orthopnea. This positional symptom occurs due to the redistribution of fluid within the lungs, leading to increased lung congestion and respiratory distress.
- Cyanosis In severe cases, patients with bronchiectasis and cyanosis present with a bluish discoloration of the skin and mucous membranes. Cyanosis occurs due to inadequate oxygenation of the blood, resulting from impaired gas exchange in the lungs.
Medical Management
History
- Respiratory Symptoms: Ask the patient about the presence and duration of symptoms such as chronic cough, excessive sputum production, shortness of breath, and recurrent respiratory infections.
- Medical History: Ask the patient about any underlying conditions predisposing to bronchiectasis, such as cystic fibrosis, prior respiratory infections, autoimmune disorders, or a history of tuberculosis.
- Environmental Exposures: Ask the patient about any potential exposure to environmental pollutants, occupational hazards, or inhalation of corrosive gases that could contribute to bronchiectasis.
- Family History: Evaluate for a family history of respiratory conditions, including cystic fibrosis or bronchiectasis, which may indicate a genetic predisposition.
- Medication History: Assess for any medications or treatments that could exacerbate or alleviate bronchiectasis symptoms, such as bronchodilators, mucolytics, or antibiotics.
Physical Examination
- Respiratory Examination: Auscultate the lungs for abnormal breath sounds such as wheezes, crackles, or diminished breath sounds. Note any signs of respiratory distress or increased difficulty breathing.
- Clubbing of Fingers: Inspect the fingertips for evidence of clubbing, characterized by bulbous enlargement and rounding of the nail beds.
- Chest Examination: Palpate the chest for tenderness or deformities. Percuss the chest to assess for dullness or hyperresonance, indicative of underlying lung pathology.
- Vital Signs: Measure vital signs, including temperature, pulse, blood pressure, and respiratory rate. Note any fever, tachycardia, or signs of hypoxia.
- General Examination: Evaluate the patient’s general appearance, including nutritional status, hydration, and signs of systemic illness such as fatigue or weight loss.
- Skin Examination: Look for signs of cyanosis or peripheral edema, which may indicate underlying respiratory compromise or cardiovascular involvement.
- Neck Examination: Examine the neck for signs of lymphadenopathy or jugular venous distention, suggestive of possible infectious or inflammatory processes affecting the respiratory system.
Investigations
- Chest X-ray: A chest X-ray will help visualize structural abnormalities in the lungs, such as bronchial dilation, thickening of bronchial walls, and areas of consolidation or atelectasis.
- High-Resolution Computed Tomography (HRCT) Scan: HRCT imaging is considered the gold standard for diagnosing bronchiectasis. It provides detailed cross-sectional images of the lungs, allowing for precise assessment of bronchial dilatation, bronchial wall thickening, and associated lung abnormalities.
- Pulmonary Function Tests (PFTs): PFTs assess lung function and may reveal obstructive or restrictive patterns characteristic of bronchiectasis. Common tests include spirometry, which measures lung volumes and airflow rates, and diffusion capacity testing, which evaluates gas exchange in the lungs.
- Sputum Culture and Sensitivity: Sputum samples should be collected and analyzed to identify the presence of bacteria, viruses, or fungi causing respiratory infections. Additionally, sensitivity testing helps determine the most effective antimicrobial agents for treatment.
- Blood Tests: Laboratory investigations such as complete blood count (CBC), inflammatory markers (e.g., C-reactive protein, erythrocyte sedimentation rate), and immunoglobulin levels may provide valuable information about the presence and severity of inflammation, infection, or immune dysfunction associated with bronchiectasis.
- Bronchoscopy: Bronchoscopy involves inserting a flexible scope into the airways to directly visualize the bronchial tree. It allows for the assessment of the bronchial mucosa, the identification of any airway abnormalities or obstructions, and collection of samples for biopsy or culture.
- Sputum Cytology: Sputum cytology involves examining sputum samples under a microscope to detect abnormal cells, which may indicate underlying lung cancer or other malignancies.
- Genetic Testing: Genetic testing may be indicated in individuals with suspected cystic fibrosis or other hereditary conditions predisposing to bronchiectasis. It helps identify specific gene mutations associated with these disorders.
- Immunological Testing: Evaluation of immune function through tests such as immunoglobulin levels, complement levels, and lymphocyte subset analysis may be warranted to assess for underlying immune deficiencies contributing to recurrent respiratory infections.
- Lung Biopsy: In certain cases, a lung biopsy may be performed to obtain tissue samples for histological examination. This procedure is typically reserved for patients with atypical or severe presentations of bronchiectasis to rule out other pulmonary diseases or complications.
Treatment
- Physiotherapy: Physiotherapy plays a crucial role in managing bronchiectasis by facilitating airway clearance and improving lung function. Breathing exercises, including deep breathing and controlled coughing techniques, help mobilize and expel mucus from the bronchial tubes.
- Postural drainage involves positioning the body to facilitate the drainage of secretions from specific lung segments, enhancing clearance. Chest percussion and vibration techniques may also be utilized to loosen mucus and promote its removal.
- High Fluid Intake: Adequate hydration is essential for individuals with bronchiectasis to help liquefy thick mucus secretions, making them easier to expectorate. Encouraging a high fluid intake, typically around 3000 milliliters per day, can aid in maintaining hydration and optimizing airway clearance.
- Antibiotic Therapy: Antibiotics are often prescribed to treat acute respiratory infections and exacerbations of bronchiectasis. The choice of antibiotic depends on the specific pathogens identified through sputum culture and sensitivity testing.
- Commonly used antibiotics include macrolides (e.g., azithromycin), cephalosporins, fluoroquinolones, and beta-lactam antibiotics. Long-term antibiotic therapy may also be considered in select cases to suppress chronic bacterial colonization and reduce the frequency of exacerbations.
- Mucolytic Agents: Mucolytic agents such as dornase alfa (Pulmozyme) may be prescribed to help thin and break down thick mucus secretions, facilitating their clearance from the airways. These medications can improve respiratory symptoms and reduce the risk of respiratory infections.
- Bronchodilators: Bronchodilators such as beta-agonists (e.g., albuterol) and anticholinergics (e.g., ipratropium bromide) may be used to alleviate bronchospasm and improve airflow in individuals with bronchiectasis. These medications help relieve symptoms such as wheezing and shortness of breath.
- Anti-inflammatory Therapy: Inhaled corticosteroids, such as fluticasone and budesonide, may be prescribed to reduce airway inflammation and suppress the inflammatory response in bronchiectasis.
- These medications help alleviate symptoms and may decrease the frequency of exacerbations in some patients.
- Surgical Intervention: Surgical removal of severely damaged or infected lung tissue may be considered in cases of localized bronchiectasis that are refractory to medical management.
- Procedures such as lobectomy (removal of a lobe of the lung) or pneumonectomy (removal of an entire lung) may be performed to improve lung function and prevent further complications.
- Immunization: Immunization against respiratory pathogens such as influenza and pneumococcus is recommended for individuals with bronchiectasis to reduce the risk of respiratory infections and exacerbations.
- Annual influenza vaccination and pneumococcal vaccination are particularly important to prevent serious complications in this population.
Nursing Management
Environment
- Ensure that there is adequate ventilation in the patient’s living space to minimize exposure to indoor pollutants and allergens.
- Implement infection control measures, including regular cleaning of surfaces and equipment, to reduce the risk of respiratory infections.
- Create a calm and relaxing environment to reduce stress and anxiety, which can exacerbate respiratory symptoms.
- Encourage smoking cessation and provide support for individuals who smoke or are exposed to secondhand smoke, as smoking can worsen bronchiectasis symptoms and disease progression.
Observation
- Monitor oxygen saturation levels using a pulse oximeter regularly. Use pulse oximetry to assess respiratory function and detect hypoxemia to act as baseline data.
- Document the frequency and severity of coughing episodes, sputum production, and any changes in respiratory symptoms.
- Assess for signs of respiratory distress, such as increased work of breathing, use of accessory muscles, or cyanosis.
- Track trends in vital signs, including temperature to rule out any infection, heart rate to rule out any heart failure, and respiratory rate to rule out respiratory failure, to identify patterns indicative of worsening bronchiectasis or acute exacerbations.
Psychological Care
- Give emotional support and active listening to the patient to address fears by explaining the process of the disease, concerns, and feelings of isolation associated with living with a chronic respiratory condition.
- Facilitate peer support groups or counseling sessions to provide opportunities for individuals with bronchiectasis to connect with others facing similar challenges.
- Educate patients and their families about bronchiectasis, its management, and coping strategies to empower them to manage the condition.
- Collaborate with mental health professionals to provide comprehensive psychological support and interventions tailored to the individual’s needs.
- Develop a therapeutic nurse patient relationship to promote trust and confidence.
Hygiene
- Educate the patients and caregivers on proper hand hygiene practices, including thorough handwashing with soap and water for at least 20 seconds.
- Provide guidance on maintaining a clean and dust-free home environment, including regular cleaning of bedding, carpets, and upholstery.
- Demonstrate proper technique for using respiratory hygiene measures, such as covering the mouth and nose when coughing or sneezing, and disposing of tissues promptly.
- Encourage adherence to vaccination schedules, including annual influenza vaccination and pneumococcal vaccination, to reduce the risk of respiratory infections.
Exercises
- Teach and encourage the performance of deep breathing exercises to promote lung expansion and improve ventilation-perfusion matching.
- Tell the patients the proper technique for postural drainage and percussion to facilitate the mobilization and clearance of respiratory secretions.
- Incorporate regular physical activity into the patient’s daily routine, focusing on exercises that improve cardiovascular fitness and strengthen respiratory muscles.
- Provide education on relaxation techniques, such as guided imagery or progressive muscle relaxation, to reduce stress and tension in the chest muscles, promoting easier breathing.
Nutrition
- Assess the patient’s nutritional status and dietary intake to identify any deficiencies or dietary modifications needed to support respiratory health.
- Collaborate with dietitians to develop individualized meal plans that are high in nutrients and calories to meet the increased energy demands associated with chronic respiratory conditions.
- Educate patients on the importance of staying hydrated and consuming adequate fluids to maintain optimal mucus viscosity and promote effective airway clearance.
- Offer nutritional counseling and support to address any dietary restrictions, food preferences, or challenges related to eating with bronchiectasis.
Elimination
- Give adequate fluid intake to prevent dehydration and maintain optimal mucus hydration for effective airway clearance.
- Provide education on dietary fiber intake and bowel habits to promote regular bowel movements and prevent constipation, which can exacerbate respiratory symptoms.
- Implement a toileting schedule to promote regular bowel habits and minimize the risk of fecal impaction, which can impair respiratory function.
- Monitor urinary output and encourage frequent voiding to prevent urinary tract infections, which can increase the risk of systemic infections and exacerbate bronchiectasis symptoms.
Medicine
- Give prescribed medications, including bronchodilators, mucolytics, and antibiotics, according to the prescribed schedule and dosage.
- Educate the patient on the purpose, dosage, and potential side effects of each medication to promote medication adherence and optimize therapeutic outcomes.
- Monitor for adverse reactions or medication interactions, and promptly report any concerns to the healthcare team for further evaluation and management.
- Collaborate with the healthcare team to adjust medication regimens as needed based on the patient’s response to treatment and changes in clinical status.
Advice at Discharge
- Give a written instructions and educational materials summarizing key self-management strategies, including medication management, airway clearance techniques, and symptom recognition.
- Schedule follow-up appointments with healthcare providers to monitor disease progression, adjust treatment plans, and address any concerns or questions.
- Coordinate referrals to community resources, support groups, or pulmonary rehabilitation programs to provide ongoing support and education beyond the hospital setting.
- Encourage patients to maintain open communication with their healthcare team and seek medical attention promptly for any worsening symptoms or concerns.
Complications of Bronchiectasis
Bronchopneumonia
- Bronchopneumonia, a type of pneumonia that affects the bronchi and surrounding lung tissue, is a common complication of bronchiectasis.
- Chronic inflammation and mucus buildup in the dilated bronchial tubes create an ideal environment for bacterial colonization and respiratory infections, predisposing individuals with bronchiectasis to recurrent episodes of bronchopneumonia.
Cor Pulmonale
- Cor pulmonale, also known as pulmonary heart disease, is a condition characterized by enlargement and dysfunction of the right side of the heart secondary to pulmonary hypertension and chronic lung disease.
- In bronchiectasis, chronic inflammation and airflow obstruction lead to pulmonary hypertension, increasing the workload on the right ventricle of the heart.
- Over time, the right ventricle may become hypertrophied and dilated, impairing its ability to pump blood effectively to the lungs, resulting in cor pulmonale.
Right-Sided Heart Failure
- Right-sided heart failure occurs when the right ventricle of the heart is unable to pump blood effectively to the lungs, leading to fluid accumulation and congestion in the systemic venous circulation.
- In bronchiectasis, chronic inflammation, hypoxia, and pulmonary hypertension contribute to the development of right-sided heart failure.
Respiratory Failure
- Severe bronchiectasis can lead to respiratory failure, a condition characterized by the inability of the respiratory system to maintain adequate gas exchange.
- Progressive airway obstruction, chronic hypoxia, and respiratory muscle fatigue contribute to respiratory failure in bronchiectasis.
Lung Abscess
- Lung abscesses can develop in individuals with bronchiectasis as a complication of recurrent respiratory infections and impaired mucus clearance.
- Pockets of pus form within the lung tissue, leading to localized inflammation, necrosis, and cavitation.
Hemoptysis
- Hemoptysis, or coughing up blood, can occur as a complication of bronchiectasis due to the presence of damaged blood vessels in the dilated bronchial tubes.
- Chronic inflammation and recurrent respiratory infections can cause erosion of blood vessels within the bronchi, leading to bleeding episodes.
Empyema
- Empyema is a serious complication of bronchiectasis characterized by the accumulation of pus in the pleural cavity surrounding the lungs.
- In bronchiectasis, persistent respiratory infections and lung abscesses can lead to the spread of infection to the pleural space, resulting in empyema.
Pulmonary Hypertension
- Pulmonary hypertension, characterized by elevated blood pressure in the pulmonary arteries, can develop as a complication of advanced bronchiectasis.
- Chronic inflammation, airway obstruction, and hypoxemia contribute to the development of pulmonary hypertension in bronchiectasis.
Lung Fibrosis
- Lung fibrosis, or the formation of scar tissue within the lung parenchyma, can occur as a consequence of chronic inflammation and recurrent respiratory infections in bronchiectasis.
- Progressive scarring and fibrosis impair lung function and gas exchange, leading to respiratory symptoms and reduced exercise tolerance.
Read more