What is a pinworm?
Pinworms, also known as Enterobius vermicularis, are small parasitic worms that commonly infect the intestines of humans, particularly children.
These worms belong to the group of parasites known as helminths and are one of the most common intestinal parasites worldwide.
Pinworm infection, or enterobiasis, is highly contagious and can spread easily from person to person, especially in crowded or unsanitary conditions.
Transmission of Pinworms
Pinworms are primarily transmitted through human-to-human contact, typically by ingesting infectious pinworm eggs or through anal insertion.
These eggs are resilient and can remain viable in a moist environment for up to three weeks.
Once deposited near the anus, pinworm eggs can easily contaminate various surfaces. The sticky surface of the eggs allows them to adhere to objects such as fingernails, hands, clothing, bedding, furniture, toys, and bathroom fixtures.
Dust containing eggs can also become airborne when disturbed, potentially entering the mouth and nose through inhalation and later being swallowed.
Although pinworms do not multiply within the human body, some larvae may hatch on the anal mucosa and migrate back into the gastrointestinal tract, a process known as retroinfection.
This retroinfection can lead to a heavy parasitic load, perpetuating the infestation. Autoinfection, where the original host becomes reinfected through either the anus-to-mouth route or retroinfection, allows pinworms to persist within the same host indefinitely.
Overall, pinworm transmission occurs through a combination of contaminated surfaces, ingestion of eggs, and the unique mechanisms of retroinfection and autoinfection, contributing to the persistence of the infestation within human hosts.
Epidemiology of Pinworm Infection
Pinworm infection, caused by Enterobius vermicularis, is widespread globally and is considered the most prevalent helminth infection.
It predominantly affects children, with finger sucking and nail biting identified as behaviors that increase both the incidence and relapse rates of infection.
Transmission occurs through contamination, making pinworms common in households and among individuals in close contact.
The prevalence of pinworm infection is not influenced by gender, social class, race, or culture. However, it is more common in families with school-aged children, primary caregivers of infected children, and institutionalized children.
Pinworm eggs, deposited around the anus by female worms, can contaminate common surfaces like hands, toys, bedding, clothing, and toilet seats.
Ingesting these eggs, either directly or indirectly, through hand-to-mouth contact or inhalation, leads to infection.
After ingestion, there is an incubation period of 1 to 2 months or longer before adult gravid female worms mature in the small intestine.
Once mature, female worms migrate to the colon and lay eggs around the anus at night, often while hosts are asleep. Infected individuals can transmit the parasite to others as long as female pinworms continue depositing eggs on the perianal skin.
Reinfection is possible through self-inoculation or exposure to eggs from another person. The primary symptom of pinworm infection, known as enterobiasis, is itching in the anal area.
Overall, pinworm infection is highly prevalent, especially among children, and transmission occurs through various routes of contamination and ingestion of eggs.
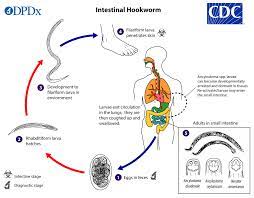
Life Cycle
The entire life cycle of pinworms, from egg to adult, occurs within the human gastrointestinal tract of a single host. The life cycle commences with the ingestion of pinworm eggs, which hatch in the duodenum.
The newly hatched larvae, measuring approximately 140 to 150 micrometers in size, rapidly grow as they migrate through the small intestine towards the colon. During this migration, the larvae undergo two molts and mature into adult pinworms.
Female pinworms typically survive for 5 to 13 weeks, while males live approximately 7 weeks. Mating between male and female pinworms occurs in the ileum, after which the male pinworms usually die and are expelled from the host via stool.
Gravid female pinworms settle in various regions of the large intestine, including the ileum, cecum, appendix, and ascending colon, where they attach themselves to the intestinal mucosa and feed on colonic contents. The gravid females become filled with eggs, with estimates ranging from about 11,000 to 16,000 eggs per female.
Egg-laying begins approximately five weeks after the initial ingestion of pinworm eggs by the human host. Gravid female pinworms migrate towards the rectum at a rate of 12 to 14 centimeters per hour.
Upon reaching the anus, the female pinworms emerge and deposit eggs onto the skin surrounding the anus through various means, including contracting and expelling eggs, disintegrating upon death, or rupturing due to host scratching.
Following egg deposition, the female pinworm becomes opaque and dies. The emergence of the female from the anus serves to obtain oxygen necessary for egg maturation.
Causes of Pinworm
- Ingestion of Pinworm Eggs: The primary cause of pinworm infection is the ingestion of pinworm eggs. These eggs are commonly found in contaminated food, water, or on surfaces touched by infected individuals.
- Direct Transmission: Pinworms are highly contagious and can spread directly from person to person through contact with contaminated hands, objects, or surfaces.
- Indirect Transmission: Pinworm eggs can also be transmitted indirectly through the ingestion or inhalation of airborne dust contaminated with eggs. This can occur when eggs are disturbed by surfaces and become airborne.
- Poor Hygiene Practices: Inadequate hand hygiene, such as not washing hands properly after using the toilet or before handling food, can contribute to the spread of pinworm infection.
- Close Contact: Pinworm infection is more common in settings where individuals live in close quarters, such as households, schools, daycares, and institutional settings, due to the ease of transmission in such environments.
- Fomite Transmission: Pinworm eggs can survive for extended periods on surfaces such as bedding, clothing, toys, and furniture. Contact with contaminated foods can lead to the transmission of the infection.
- Autoinfection: In some cases, individuals can become reinfected with pinworms by ingesting eggs that were previously expelled from their own bodies. This autoinfection can occur through activities such as scratching the anal area and then touching the mouth without proper hand hygiene.
Signs and Symptoms
- Anal Itching: The most common symptom of pinworm infection is intense itching around the anus, particularly at night. This itching is caused by the movement of female pinworms as they lay eggs around the anal area.
- Restlessness: Infected individuals may experience restlessness, especially at night, due to discomfort caused by anal itching.
- Difficulty Sleeping: The itching sensation around the anus can disrupt sleep patterns, leading to difficulty falling asleep or staying asleep throughout the night.
- Irritability: Chronic itching and disrupted sleep can contribute to irritability and mood changes, particularly in children.
- Abdominal Pain: Some individuals may experience mild abdominal pain or discomfort, although this symptom is less common than anal itching.
- Loss of Appetite: In severe cases of pinworm infection, loss of appetite may occur, possibly due to discomfort or gastrointestinal disturbances.
- Secondary Infections: Excessive scratching of the anal area can lead to skin irritation, inflammation, and secondary bacterial infections.
- Vaginal Itching: In females, pinworms may migrate to the vaginal area, causing itching and discomfort.
- Bedwetting: Pinworm infection may contribute to bedwetting, particularly in children, due to disrupted sleep patterns and discomfort.
- Weight Loss: Severe and prolonged pinworm infections may result in weight loss, although this is rare and usually associated with complications such as malnutrition.
Medical Management
Patient History
- Ask about any symptoms such as anal itching, particularly at night, restlessness, difficulty sleeping, abdominal pain, and irritability.
- Ask about recent exposures to potential sources of infection, such as contact with individuals known to have pinworm infection or exposure to contaminated surfaces or environments.
- Explore any history of previous pinworm infections or treatments.
Physical Examination
- Inspect the perianal area for signs of inflammation, redness, or excoriation due to scratching.
- Look for visible evidence of pinworms or their eggs around the anus, such as tiny white threads or specks.
- Check for signs of secondary bacterial skin infections resulting from excessive scratching.
- Assess for any abdominal tenderness or discomfort that may indicate a more severe infection or complications.
Additional Considerations
- In pediatric patients, ask about symptoms such as irritability, difficulty concentrating, or changes in behavior that may indicate pinworm infection.
- Consider performing a scotch tape test or cellophane tape test to collect samples from the perianal area for microscopic examination to confirm the presence of pinworm eggs.
- Discuss the possibility of household or close contacts also undergoing screening and treatment if warranted based on history and examination findings.
- Rule out other potential causes of anal itching or gastrointestinal symptoms, such as other parasitic infections, dermatological conditions, or gastrointestinal disorders.
Investigations
- Scotch Tape Test: This simple and non-invasive test involves pressing a piece of clear adhesive tape against the skin around the anus in the morning before bathing or using the toilet. The tape is then transferred to a glass slide and examined under a microscope for the presence of pinworm eggs.
- Stool Examination: In some cases, a stool sample may be collected from the patient and examined for the presence of pinworm eggs or adult worms. This can be particularly useful if the infection is suspected to be more severe or if other gastrointestinal symptoms are present.
- Perianal Swab: A cotton swab may be used to collect samples from the perianal area for microscopic examination to detect pinworm eggs or evidence of infection.
- Serological Tests: While less commonly used, serological tests may be performed to detect antibodies against pinworm antigens in blood samples. These tests are not routinely recommended for diagnosis but may be useful in certain situations, such as when other methods are inconclusive or to monitor response to treatment.
- Diagnostic Imaging: In rare cases where complications of pinworm infection are suspected, such as intestinal obstruction or appendicitis, diagnostic imaging studies such as abdominal ultrasound or computed tomography (CT) scan may be performed to assess the extent of the infection and associated complications.
Treatment
- Secondary Bacterial Infections: Excessive scratching of the perianal area due to itching caused by pinworm infection can lead to skin irritation and breakdown, increasing the risk of bacterial infections such as cellulitis or impetigo.
- Sleep Disturbance: Persistent itching, particularly at night when female pinworms lay their eggs, can disrupt sleep patterns and lead to insomnia or poor quality sleep, impacting overall well-being and daily functioning.
- Psychological Distress: Chronic or recurrent pinworm infection can cause psychological distress, including anxiety, embarrassment, and social isolation, especially in children and adolescents.
- Complications in Rare Cases: Although rare, severe complications of pinworm infection may include appendicitis, urinary tract infections, or vaginal infections (in females) due to the migration of pinworms to other parts of the body.
- Chronic Infection: If left untreated or inadequately managed, pinworm infection can become chronic, leading to persistent symptoms and complications over time.
- Recurrent Infections: Despite treatment, some individuals may experience recurrent pinworm infections, especially in settings where hygiene measures are inadequate or reinfection occurs due to close contact with infected individuals.
- Impact on Quality of Life: Pinworm infection and its associated symptoms, such as anal itching and sleep disturbances, can significantly impact an individual’s quality of life, leading to discomfort, frustration, and reduced overall well-being.
- Transmission to Others: Failure to control pinworm infection can result in transmission to other household members, caregivers, or close contacts, leading to outbreaks within communities or institutions.