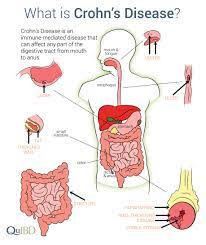
Cholera is a bacterial infection caused by the bacterium Vibrio cholerae. It typically spreads through contaminated water and food, particularly in areas with poor sanitation and hygiene practices. Cholera can lead to severe diarrhea and dehydration, and in severe cases, it can be life-threatening if not promptly treated. Symptoms of cholera include profuse, watery diarrhea, vomiting, and muscle cramps. Treatment usually involves rehydration therapy, including oral rehydration solution (ORS) or intravenous fluids, along with antibiotics to shorten the duration of illness and reduce the severity of symptoms. Prevention strategies include improving sanitation, ensuring access to clean drinking water, and promoting good hygiene practices such as handwashing. Vaccines are also available to provide protection against cholera in high-risk populations.
Incubation Period: Cholera has an incubation period ranging from a few hours to up to 5 days. During this time, individuals may be infected with the Vibrio cholerae bacterium but not yet display symptoms.
Transmission: The primary mode of transmission for cholera is the oral-fecal route, typically occurring through the ingestion of contaminated food and water. Poor sanitation and hygiene practices contribute to the spread of the disease, particularly in areas with inadequate access to clean water and sanitation facilities.
Causative Organism
Cholera is caused by the bacterium Vibrio cholerae. There are two main biotypes:
- Classical cholerae vibrio: This biotype of Vibrio cholerae is responsible for the majority of cholera cases worldwide.
- Haemolytic El Tor vibrio: This biotype is a variant of Vibrio cholerae that emerged in the 20th century and is associated with some cholera outbreaks.
Characteristics of Vibrio Cholerae:
- Shape: Vibrio cholerae is characterized by its comma shape, resembling a curved rod.
- Oxygen Requirement: It is an aerobic organism, meaning it requires oxygen to survive and grow.
- Gram Stain: Vibrio cholerae is Gram-negative, indicating that it does not retain the crystal violet stain in the Gram staining process.
- Spore Formation: It does not form spores, distinguishing it from certain other bacteria that can produce spores for survival.
- Motility: Vibrio cholerae is a motile organism, possessing both flagella and somatic antigens that enable it to move actively.
- Heat and Disinfectant Sensitivity: It is susceptible to heat, being killed at temperatures of 55°C for 15 minutes. Additionally, it can be effectively eliminated by phenolic and hypochlorite disinfectants.
- Environmental Survival: Vibrio cholerae can survive in aquatic environments for extended periods, entering a dormant state that allows it to persist until conditions become favorable for growth and reproduction.
Epidemiology:
Cholera predominantly affects individuals from low socioeconomic backgrounds residing in areas with poor sanitation, limited access to healthcare services, and unsafe water supplies. The disease is particularly prevalent in regions of Asia and Africa where these conditions are widespread. Cholera transmission occurs primarily through the ingestion of contaminated feces and water. Additionally, consumption of other perishable foods such as milk, cold-cooked dishes, and unwashed fruits and vegetables can also contribute to the spread of infection.
Pathogenesis:
Vibrio cholerae primarily resides in the gut and does not enter the bloodstream. It attaches to the mucosa of the small intestines using outer membrane proteins and flagella adhesions. The bacterium produces an enterotoxin that leads to excessive loss of fluid and electrolytes. This enterotoxin inhibits the absorption of sodium chloride, leading to its excretion along with water, potassium, and bicarbonate. Natural infection typically results in immunity to both the cholera toxin and bacterial surface antigens.
Signs and symptoms:
Evacuation Phase:
- Onset of diarrhea ranging from mild to acute, initially containing fecal matter but later becoming watery, often described as “rice water stool.”
- Projectile vomiting may accompany diarrhea.
- Severe dehydration occurs due to extensive fluid loss from diarrhea and vomiting.
Collapse Phase:
- Muscle cramps develop due to electrolyte imbalances resulting from fluid loss.
- Metabolic acidosis manifests with signs of air hunger, characterized by deep and sometimes rapid breathing.
- Hypovolemic shock ensues due to vascular depletion, leading to vascular collapse. Symptoms include hypotension, tachycardia, and impalpable pulses at the wrist, along with cold, clammy skin, and oliguria. Without intervention, shock can progress to acute renal failure and, potentially, death.
Recovery Phase:
As the patient enters the recovery phase, there is a noticeable improvement in their condition, and the signs and symptoms begin to subside.
- Resolution of Symptoms: The diarrhea and vomiting gradually diminish, and the patient experiences a reduction in the severity and frequency of bowel movements and episodes of vomiting.
- Hydration Restoration: With appropriate rehydration therapy and fluid replacement, the patient’s hydration status improves. Intravenous fluids or oral rehydration solutions help replenish lost fluids and electrolytes, aiding in the restoration of normal hydration levels.
- Regaining Strength: The patient starts to regain strength and energy as they recover from the debilitating effects of dehydration and metabolic disturbances. Muscle weakness and fatigue begin to diminish, allowing the patient to resume normal activities gradually.
- Normalization of Vital Signs: Vital signs, such as blood pressure, heart rate, and respiratory rate, stabilize and return to normal ranges as the patient’s condition improves.
- Resumption of Appetite: As the gastrointestinal symptoms subside, the patient’s appetite typically returns. They may start to tolerate oral intake better and resume eating a normal diet.
Diagnosis:
Clinical Diagnosis in Epidemics: In epidemic situations, a presumptive diagnosis of cholera is often based on clinical presentation or epidemiological factors. For instance, individuals aged 5 years or older who develop acute watery diarrhea with or without vomiting, particularly in areas where cholera outbreaks are likely to occur, may be clinically diagnosed with the disease.
Laboratory Diagnosis:
- Dark Field Microscopy: Examination of stool samples under dark field microscopy may reveal the characteristic darting movement of Vibrio cholerae. Inhibition of this movement by specific antisera (e.g., O1 antisera) provides strong supportive evidence for the diagnosis.
- Microbiological Culture: Stool, vomitus, or rectal swabs are collected for microbiological culture and sensitivity testing. This method confirms the presence of Vibrio cholerae in the samples, aiding in a definitive diagnosis.
- Immunofluorescent Assay: Immunofluorescent techniques allow for rapid diagnosis of cholera by detecting specific antigens associated with Vibrio cholerae in clinical specimens. This method offers a quick and efficient means of confirming the presence of the bacteria.
Management
Aims:
- Correcting Fluid and Electrolyte Imbalance: The primary aim is to restore normal fluid and electrolyte levels in the body to mitigate the effects of dehydration and electrolyte disturbances.
- Eliminating the Causative Organism: Efforts are focused on eradicating the Vibrio cholerae bacterium from the body to halt the progression of the disease and prevent further transmission.
- Preventing the Spread of Infection: Implementation of measures to contain and control the spread of cholera, including isolation of affected individuals, proper sanitation practices, and hygiene protocols to minimize the risk of transmission to others.
- Preventing Complications from Fluid and Electrolyte Loss: Proactive measures are taken to prevent and manage complications arising from severe dehydration and electrolyte imbalances, such as hypovolemic shock, metabolic acidosis, and organ failure. This involves prompt rehydration therapy and close monitoring of the patient’s clinical status.
Therapy:
Correction of Fluid and Electrolyte Imbalance: Immediate initiation of intravenous fluid therapy is essential for correcting fluid and electrolyte imbalances. Use fluids such as Ringer’s lactate or normal saline. If the patient is able to drink, administer oral rehydration solution (ORS) while setting up the intravenous drip.
In cases of severe dehydration, administer rapid intravenous fluid resuscitation, giving 30 mL/kg body weight within the first 30 minutes, followed by 70 mL/kg body weight over the next 2½ hours. The goal is to restore normal hydration and acid-base balance within 2-3 hours. Subsequently, continue rehydrating the patient at a slower rate until the pulse and blood pressure return to normal.
Once the patient is capable of oral intake, provide oral rehydration at a rate of 5 mL/kg body weight per hour (250 mL/hr). Monitor vital signs every 30 minutes during fluid resuscitation, adjusting the rate of infusion if signs of circulatory overload are observed.
Monitor urine output hourly, aiming for a normal range of 30–40 ml/hr. If urine output is reduced, indicating potential acute renal failure, prompt medical intervention is necessary.
Administer ORS as soon as the patient is able to drink orally. Maintain fluid replacement by accounting for losses from stool. Oral rehydration should be encouraged and administered as needed.
Antimicrobial Agents:
- Tetracycline: Administer 500mg orally four times a day for a duration of three days. Tetracycline is effective in treating cholera and helps eradicate Vibrio cholerae from the body.
- Doxycycline: A single dose of 300mg is considered the drug of choice for cholera treatment. Doxycycline exhibits potent antibacterial activity against Vibrio cholerae and aids in resolving the infection.
- Cotrimoxazole: Prescribe 960mg orally twice daily for a duration of three days. Cotrimoxazole, a combination of sulfamethoxazole and trimethoprim, is another option for treating cholera effectively.
- Ciprofloxacin: Administer 500mg orally twice daily for three days. Ciprofloxacin is a broad-spectrum antibiotic with activity against Vibrio cholerae, making it suitable for cholera treatment.
- Erythromycin: Prescribe 500mg orally four times a day for three days. Erythromycin is effective in treating cholera and can be used as an alternative antimicrobial agent in cases where other antibiotics are not suitable.
These antimicrobial agents help eliminate the causative organism, Vibrio cholerae, from the body, contributing to the resolution of cholera infection and preventing its complications. It is crucial to adhere to the prescribed dosage and duration of treatment to ensure effectiveness and minimize the risk of antimicrobial resistance.
Nursing Management
Patient Isolation:
- Implement strict isolation protocols to prevent the spread of infections to other patients and healthcare workers.
- Ensure the patient is placed in a designated isolation room with appropriate signage to alert staff and visitors.
- Provide personal protective equipment (PPE) to all healthcare workers entering the isolation area.
- Limit visitors and ensure they adhere to infection control measures, such as hand hygiene and wearing PPE.
- Educate the patient and family members on the importance of isolation and adherence to infection control practices.
Infection Prevention:
- Emphasize the importance of hand hygiene to the patient, family members, and healthcare staff, promoting regular handwashing with soap and water or alcohol-based hand sanitizer.
- Ensure proper disposal of contaminated materials and disinfection of patient care areas.
- Educate the patient and family members on respiratory hygiene, including covering coughs and sneezes with a tissue or elbow.
- Implement environmental cleaning protocols to maintain a clean and sanitized patient care environment.
- Monitor and enforce adherence to infection prevention practices among healthcare staff through regular audits and education sessions.
Disease Notification:
- Ensure timely reporting of suspected or confirmed cases of the disease to public health authorities as per local regulations.
- Facilitate contact-tracing activities by providing relevant information about the patient’s contacts and potential exposure sources.
- Collaborate with public health officials to implement control measures, such as quarantine or community outreach programs.
- Educate the patient and family members on the importance of disease notification and cooperation with public health authorities.
- Maintain the confidentiality and privacy of patient information while complying with reporting requirements.
Fluid Therapy:
- Assess the patient’s fluid status and electrolyte levels regularly to guide fluid therapy interventions.
- Administer intravenous fluids as prescribed, ensuring accurate calculations of fluid rates and electrolyte composition.
- Monitor the patient’s response to fluid therapy, including vital signs, urine output, and clinical signs of dehydration or fluid overload.
- Adjust the fluid therapy regimen based on ongoing assessment findings and the patient’s clinical status.
- Educate the patient and family members on the importance of fluid intake and adherence to the prescribed fluid therapy regimen.
Observation:
- Conduct frequent assessments of the patient’s vital signs, including temperature, pulse, respiratory rate, and blood pressure.
- Monitor the patient’s level of consciousness and mental status, noting any changes or signs of deterioration.
- Document intake and output accurately, including fluid intake, urine output, and any losses from vomiting or diarrhea.
- Perform regular physical assessments to monitor for signs of complications or deterioration in the patient’s condition.
- Communicate and collaborate with other members of the healthcare team to ensure comprehensive observation and monitoring of the patient.
Psychological Care:
- Provide emotional support and reassurance to the patient and family members, addressing fears and concerns about the disease and its treatment.
- Encourage open communication and active listening, allowing the patient to express their feelings and concerns.
- Offer information and education about the disease process, treatment options, and expected outcomes to alleviate anxiety and uncertainty.
- Facilitate access to pastoral care services or mental health support for patients experiencing emotional distress or psychological symptoms.
- Collaborate with the interdisciplinary team to develop and implement individualized care plans that address the patient’s psychosocial needs and promote coping strategies.
Hygiene:
- Assist the patient with personal hygiene activities, including bathing, oral care, and toileting, as needed.
- Ensure proper disposal of contaminated materials, such as soiled linens and medical waste, in accordance with infection control protocols.
- Educate the patient and family members on hand hygiene practices, including proper handwashing techniques and the use of hand sanitizer.
- Maintain a clean and sanitized patient care environment, including regular cleaning and disinfection of patient rooms and equipment.
- Implement standard precautions and transmission-based precautions as appropriate to prevent the spread of infection.
Nutrition:
- Assess the patient’s nutritional status and dietary intake, identifying any deficiencies or special dietary needs.
- Offer small, frequent meals and snacks that are easily digestible and well-tolerated by the patient.
- Encourage oral fluid intake to prevent dehydration, offering oral rehydration solutions or flavored beverages as tolerated.
- Collaborate with the dietitian to develop individualized meal plans that meet the patient’s nutritional requirements and preferences.
- Monitor the patient’s weight and nutritional status regularly, adjusting dietary interventions as needed to optimize nutritional intake and support recovery.
Advice for Home:
- Provide education and instructions on post-discharge care, including medication management, wound care, and follow-up appointments.
- Review signs and symptoms of complications or worsening illnesses that require prompt medical attention, such as persistent fever or difficulty breathing.
- Encourage the patient and family members to maintain good hygiene practices at home, including handwashing, surface cleaning, and proper food handling.
- Provide resources and referrals to community support services or home health agencies, if needed, to assist with ongoing care and support.
- Offer emotional support and encouragement to the patient and family members during the transition from hospital to home care, addressing any concerns or questions they may have.
Prevention and Control of Cholera:
- Proper Waste Disposal: Effective disposal and treatment of fecal waste contaminated with cholera bacteria, along with clothing and bedding that have come into contact with it, are paramount to preventing the spread of the disease.
- Sewage Management: Treatment of sewage before its discharge into waterways or underground water sources helps prevent potential undetected cholera patients from transmitting the disease through contaminated water.
- Source Protection: Posting warnings near contaminated water sources, along with guidelines on how to decontaminate water, helps alert individuals to the presence of cholera and mitigate the risk of infection.
- Water Sterilization: Boiling, filtering, and chlorinating water are effective methods for killing cholera bacteria and preventing the spread of infection. All materials that come into contact with cholera patients, including clothing and bedding, should be sterilized with hot water and, if possible, chlorine bleach. Hands and other body parts that touch cholera patients or their belongings should be thoroughly cleaned and sterilized. All water used for drinking, washing, or cooking should undergo sterilization by boiling or chlorination, especially in areas where cholera is prevalent.
- Improving Water Supply and Sanitation: Enhancing access to clean water and proper sanitation facilities helps reduce the risk of cholera transmission.
- Contact Tracing: Identifying and monitoring individuals who have come into contact with cholera patients helps prevent further spread of the disease.
- Personal Hygiene: Promoting good personal hygiene practices, such as regular handwashing, is essential for preventing cholera transmission.
- Postponing Festivals and Gatherings: Temporarily postponing large gatherings and festivals can help limit opportunities for cholera transmission in communities.
- Behavioral Changes: Encouraging behavioral changes, such as washing hands, boiling water, heating food before consumption, and using toilets or latrines, is crucial for preventing cholera infection.
- Adequate Case Treatment: Providing prompt and appropriate treatment to individuals diagnosed with cholera is vital for reducing morbidity and mortality associated with the disease.
- Active Case Reporting: Prompt reporting of suspected cholera cases in areas where the disease was previously not present facilitates early detection and intervention to prevent its spread.
Complications of Cholera:
- Paralytic Ileus: Cholera can lead to paralysis of the intestines, resulting in a condition known as paralytic ileus, which disrupts normal bowel function and can cause severe abdominal discomfort and distension.
- Muscle Weakness: Dehydration and electrolyte imbalances associated with cholera may lead to muscle weakness, which can affect mobility and overall physical strength.
- Cardiac Arrhythmias: Electrolyte disturbances, particularly potassium imbalances, can predispose individuals with cholera to develop irregular heart rhythms or cardiac arrhythmias, which may pose serious cardiac complications.
- Renal Failure: Severe dehydration and hypovolemia can compromise kidney function, leading to acute renal failure, characterized by a significant decrease in urine output and impaired kidney function.
- Metabolic Acidosis: Loss of bicarbonate ions through diarrhea and vomiting can result in metabolic acidosis, a condition characterized by an imbalance in the body’s acid-base equilibrium, leading to acidification of the blood and tissues.
- Hypoglycemia: Prolonged fasting and decreased oral intake in individuals with cholera can lead to low blood sugar levels, known as hypoglycemia, which may manifest as weakness, confusion, and even loss of consciousness if left untreated.
- Pulmonary Edema: In severe cases of cholera, fluid overload resulting from aggressive fluid resuscitation or electrolyte imbalances may lead to pulmonary edema, a condition characterized by the accumulation of fluid in the lungs, causing respiratory distress and compromised oxygenation.